Nutrition and Feeding after discharge from the Neonatal Unit
Feeding is so much more than just provision of nutrients, it will help build a relationship and bond with your baby. This page aims to explain the feeding journey your baby might have when they go home from the neonatal unit.
Oral feeding
Your baby might be ready to start oral feeds, e.g. breastfeeding or bottles, when it starts showing hunger cues and wake around feed times. These can be individual to your baby, but most might start off by being more awake during feed time, rooting and opening their mouth, putting hands to mouth (see the picture below). Crying is usually a late cue that they’re hungry – if they do get to this stage it might be worth comforting them first and then offering a feed.
Some babies might start their oral feeding journey with non-nutritive sucking, this might include offering an expressed breast or a dummy or a gloved finger – this can help babies develop the skill of sucking, without having to swallow milk as they might not be developmentally ready to do so yet or their respiratory support might prevent safe swallowing/feeding.
Establishing breastfeeding
There are many benefits to breastfeeding your baby but it can take some time to establish with a preterm baby so try not to get discouraged if this is your preferred way of feeding.
It is not unusual to use formula alongside EBM or breastfeeding. This is common if there is insufficient maternal milk supply or if parents wish to stop expressing it. You can offer your milk +/- formula in a bottle.
However if you intend to breastfeed your baby we would recommend that you aim to establish this first for a minimum of 1-3 weeks before you consider introducing bottles. This is because the mechanics of feeding from the breast and bottle are very different and experience tells us that babies who start having bottles before or when establishing breastfeeding can struggle to do so effectively.
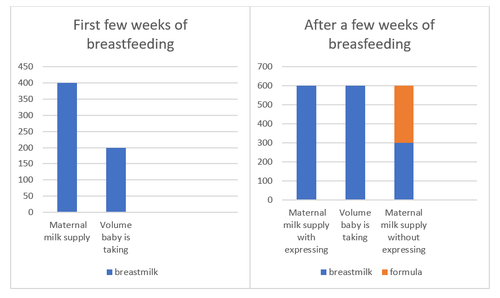
We would advise that you express your milk after breastfeeds whilst your baby learns to take more milk, which will support establishing a good milk supply for when your baby is ready to take more.
The table below shows that initially, your milk supply might be better than what your baby can take. However, if you don’t express, the breasts will stop producing as much milk, whilst your baby learns to take more milk. If mums are not expressing their milk in the first few weeks, they might find that they don’t have enough milk to meet the baby’s needs after a few weeks and may have to top up with formula as a result to support baby’s growth.
It might take some time until the baby can take sufficient volume to support their growth and it is not unusual for baby’s growth to slow down or for the baby to lose some weight in this transition period. However, we would expect their weight to start tracking a centile line after about a week or so (no longer than a couple of weeks).
In case of difficulties:
If your baby is struggling to gain weight we might need to look more closely into
- baby’s ability to suck/swallow, their behaviour on the breast (are they getting frustrated, struggling to latch etc.),
- their endurance on the breast (how long they can actively feed),
- your milk supply (e.g. if your breast feels empty and baby still looking for milk, if baby is struggling to get milk)
Expressing and feeding your baby can be difficult to coordinate therefore it’s advised that you have support from your midwife, health visitor, and most importantly a partner or family/friends for those first few weeks when you establish supply.
However, long term, you might find that breastfeeding requires less effort than feeding expressed milk or preparing formula.
If you’re concerned that your baby is struggling with establishing breastfeeding ask to speak to an Infant feeding specialist nurse, health visitor, local breastfeeding support group or GP if you’re concerned about their growth.
Formula
When breastmilk is not available or you choose not to breastfeed, your baby will require formula to meet their nutritional needs. Formula can also be used alongside your milk. There are different types of formula we use on the unit and after your baby is discharged home. Your baby might be discharged on one type of formula or a combination of different formulae and/or breastmilk.
| Formula used for preterm babies | Is it prescribed? | Calories per 100ml | Do they need vitamins and iron?* | How long do they need it? |
|---|---|---|---|---|
| Nutriprem 2® (or SMA Goldprem 2®) | Yes | 72kcal |
No (Yes, if majority of feeds are maternal milk or term formula) |
Depends on growth but can be used till 12months corrected age |
| Standard/term “First” formula | No | 68kcal | Yes |
Around 12 months corrected age if baby is taking a good variety of foods |
| Infatrini® or SMA High Energy® | Yes | 100kcal | Yes (No, if majority of feeds are preterm formula) |
Depends on growth, but can continue till 18months corrected age |
*Babies born < 34 weeks will need to start on additional vitamins and iron (usually Abidec® and Sytron®) when having standard formula or breastmilk. These would normally continue until at least 6 months corrected age but can be offered until 12 months corrected age, especially if baby struggles with introducing a wide variety of foods in their diet.
You can find more information on baby milk, including safe preparation and safe bottle feeding on the First Steps Nutrition website.
Growth
As babies get closer to their due date (term) their nutritional requirements tend to reduce. They might not need as many calories, protein and vitamins/minerals as they did when they were first born.
As they get closer to term, their growth might start to go up the centile lines and changes to their feeds might be made, e.g. stopping breastmilk fortifier, changing from Nutriprem 1® to Nutriprem 2®, etc. However, a lot of other things might be happening around the same time, e.g. weaning off respiratory support/oxygen, coming out of hot cots, stopping NG feeds, and relying more on responsive breastfeeds – all of these things can impact their growth. Your neonatal team will bear this in mind and you will agree on the best time to step down to feeds you can go home on (you can’t go home on breastmilk fortifier or Nutriprem 1®).
It is important to continue to review your baby’s growth when home – your health visitor might be able to come out and weight your baby at home or you can go to your local health visiting Hub to have your baby weighed.
Those plots are then compared against a line of expected growth pattern (AKA a centile line).
You can learn more about growth charts here
What if babies are deviating away from their centile line?
- If the pattern of growth trends down and keeps crossing centile lines downward that would be an indication of poor growth and an indication that baby might need some support, this can be around breastfeeding/expressing practices, general feeding practices (e.g. frequency of feeds) or thinking about higher energy formula.
- If the pattern of growth follows a centile line it would mostly likely indicate good growth. It’s probably best to continue the current feeding plan.
- If the pattern of growth crosses centiles in the upward direction the pattern of growth might be optimal (this might be true if baby is catching up following weight loss) or it could be excessive (especially if crossing above birth centile) – this might be an indication that the nutrition they’re receiving is too much for their needs and perhaps ready to step down to a more appropriate feeding plan for them, e.g. stop high energy milk, or change from preterm discharge formula, (e.g. Nutriprem 2®) to regular term formula – if this is the case bear in mind they might need to start vitamins* if they were born at <34 weeks.
Make sure to ask your neonatal team to show you your baby’s growth chart so that you can see for yourself.
Lots of things can affect growth. The most obvious is getting enough calories and protein from their milk. If it is thought that baby is managing to take optimal volumes of milk and your milk supply is good but baby is still not gaining weight this might need to be investigated further.
There are some less obvious reasons why a baby’s growth might be slow, e.g. low tissue sodium or zinc, underlying conditions like hypothyroidism or treatment for certain conditions like steroids. It might be worth considering these if your baby is still struggling to grow on what would seem an optimal milk regimen – your neonatal team or health visitor can discuss this with you.
Babies after abdominal surgery
Some babies have to have surgery to repair or remove damaged parts of the gut. Depending on the amount of gut that was removed, their ability to absorb nutrients from their feed might be affected. Therefore, babies that have had surgery on their gut are at an even higher risk of poor growth and nutrition. They are more likely to have low sodium (especially if they had high losses through a stoma) and more likely to need larger feed volumes and/or specialist formula (see below) to support nutrition, ideally alongside maternal breast milk.
Maternal breastmilk is still the best choice for any baby, whether soon after surgery or later down the line, it will help them heal. However, due to their increased requirements, they might need some support from formula or breastmilk fortifier – your neonatal team will be able to advise around this.
| Specialist formula | Is it prescribed? | Calories per 100ml | Do they need vitamins and iron?* | How long do they need it? |
|---|---|---|---|---|
| Aptamil Pepti Junior® (may be concentrated) | Yes | 68kcal (can be concentrated to up to 100kcal) |
Yes (No if concentrated) |
Depends on growth and tolerance. |
| Infatrini Peptisorb® | Yes | 100kcal | Yes |
Depends on growth, but can continue till 18months corrected age. |
Monitoring
Going home can be an extremely exciting time that you might have been waiting for since your baby was born, but it can come with mixed emotions.
It is important to continue to review your baby’s growth when home – your health visitor might be able to come out and weigh your baby at home or you can go to your local health visiting Hub to have your baby weighed.
You might want to start with weekly weights for the first 2-4 weeks and if growth is satisfactory (see “growth” section above) you might want to reduce it to every 1-3 months.
You can ask your neonatal team to give you a growth chart and show you how to plot your baby – you can also print them from the RCPCH website.
Weaning to solids
You might hear lots of conflicting information about when is the best time to start offering solid foods to your preterm baby. In truth, your baby will tell you. You just need to learn how to pick up on their cues.
Each baby is different and will have had their own journey with feeding.
Most importantly do not push your baby if they seem hesitant it can do more harm than good.
Try to make it a fun, messy, and enjoyable experience for them.
Do your reading – starting too early or progressing too quickly can set them back or trigger oral hypersensitivity.
Once you feel your baby is ready (take a look at the readiness quiz!) or almost ready, you could start by offering very small (ice cube sized) amounts of smooth purees for them to play with either on the floor, in a high chair, or sitting in your arms – use this experience to have fun and enjoy exploring, rather than eat. You can also offer a baby spoon for the baby to hold and play with safely. This can be a gentle way to start your journey with solids until the baby is showing all readiness cues.
The Bliss website offers comprehensive information on starting solids.
The Solid Starts® app might help you navigate what is suitable for different age groups – however, take this information with a pinch of salt as every baby is different and some will only enjoy purees whilst others want to explore finger foods. Follow your baby’s cues. But be mindful that you might need to introduce/try a new food a few times before your baby might accept it – this is normal.
If they are gagging regularly on finger foods, it might be best to hold back on these and only offer foods that they can manage more easily, and perhaps starting with ‘bite and dissolve’ foods when trying finger foods – over time you should be able to offer more finger foods as your baby learns how to manage these in their mouth.
If your baby has been found to have difficulties with swallowing/managing oral intake speak with your Speech and Language therapist before starting weaning.