Growth Hormone (GH)
Chemical Pathology
Notes
- Growth hormone (GH) is secreted from the anterior pituitary. The hormone has several isoforms, the most abundant being the 22 kDa form. Both the 22 kDa form and the 20 kDa form are measured by the local assay.
- GH secretion is stimulated by growth hormone releasing hormone (GHRH), hypoglycaemia, insulin, ghrelin and exercise; release is suppressed by hyperglycaemia, somatostatin and drugs, such as beta-blockers.
- GH is vital for the normal growth of bones during childhood, but also helps maintain normal metabolism in children and adults through its anabolic effects that increase glucose uptake, protein synthesis and lipolysis.
- GH deficiency is the most common endocrine cause of short stature, but also exhibits in adults as reduced muscle strength and bone mass, and impaired cardiac function. The deficiency may occur as an isolated hormonal deficiency or with deficiencies in other pituitary hormones arising from hypopituitarism, tumours in the central nervous system, cranial irradiation or other physiological causes. In about half of the children with GH deficiency, the cause is unknown (idiopathic growth hormone deficiency).
- GH excess is usually caused by a growth hormone-secreting tumour of the pituitary. Gigantism is when the excess secretion occurs in childhood, whereas acromegaly is when the excess secretion occurs in adulthood.
- Stimulation or suppression tests are needed to assess a growth hormone disorder, with baseline and post-stimulation or post-suppression samples taken. Random testing is rarely helpful.
Sample requirements
- If patient on high dose biotin therapy (>5mg/day) collect sample at least 8 hours after the last dose.
- Assay unsuitable if patient receiving pegvisomant therapy due to interference.
- Assay unsuitable in pregnancy due to cross-reactivity with placental growth hormone.
- Samples for dynamic function tests must all be collected in the tube type.
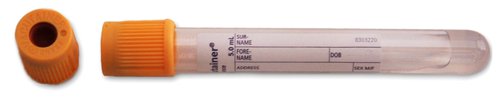
For adults, blood taken into a 5mL gold top gel tube (or rust top for the Acute Unit)
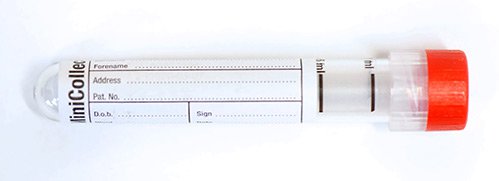
For children, blood taken into a 3.5mL rust top tube

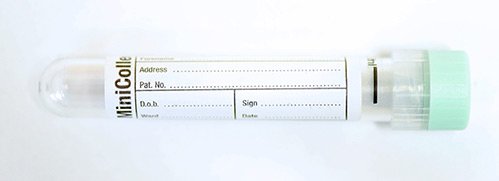
For neonates, blood taken into a 1ml minicollect plain tube or 1mL minicollect lithium heparin tube
Storage/transport
Do not store. Send at ambient temperature to the laboratory on the day of sample collection.
Required information
Relevant clinical details including reason for the request.
Samples collected during stimulation tests should be clearly labelled with the date and time and order of collection and the details of the test should be indicated on the request form.
Turnaround times
Samples are analysed in weekly batches with results available within 8 days.
Reference ranges
- Reference ranges are not reported with GH results.
- Cut-off levels for the diagnosis of GH deficiency or excess depend on the stimulation or suppression test and other factors, such as the patient’s body mass index, and should be used in conjunction with clinical-auxological criteria and NMR imaging of the pituitary gland.
- GH secretion is normally pulsatile, and varies with age, sex and many external and internal factors. Results should therefore be interpreted with care and random GH tests are rarely useful.
- GH levels are reported in ug/L
Further information
Page last updated 18/12/2024