Theophylline
Chemical Pathology
Notes
Theophylline is an oral bronchodilator with a narrow therapeutic window, used in the treatment of conditions such as asthma and chronic obstructive pulmonary disease (COPD).
Theophylline also has CNS stimulant properties, increasing the respiratory drive in hypoxia and this effect is sometimes used in the treatment of apnoea in premature neonates. Theophylline is partly metabolised to caffeine in neonates and caffeine citrate is more often used directly now as this causes less side effects compared to administering the parent drug.
- Theophylline is rapidly absorbed from the gastrointestinal tract when administered in liquid form or as uncoated tablets, with peak concentrations occuring within 1 - 2 hours of a single dose on an empty stomach.
- Peak concentrations are delayed up to 6 - 10 hours after food or if sustained release products are used.
- A small fraction is excreted unchanged in the urine but most of the drug is first metabolised in the liver with urinary excretion of the metabolites 1,3 dimethyluric, 1-methyluric acid and 3-methlyxanthine.
- Many factors affect the rate of theophylline metabolism. Concentrations are increased in heart failure, cirrhosis, viral infections and in the elderly, and decreased in smokers, chronic alcoholics and by drugs that induce hepatic metabolism, resulting in a wide range of elimination half-lives in different patient groups. In normal adults the half-life averages 6-9 hours.
- Some formulations contain theophylline salts, for example with ethylenediamine which is then known as aminophylline. The increased soluability of aminophyline compared to theophylline is an advantage for intravenous use.
Theophylline levels are useful for optimising dosing. Monitoring is also valuable in confirming a diagnosis of theophylline toxicity and in managing the overdosed patient.
Sample requirements
- For oral dosing, samples should be taken at least five half-lives after any change in dose. For adults this is 3 days; for children 2 days and for neonates 7 days.
- The recommended sampling time for monitoring of modified release preparations that are given every 12 hours is 4 - 6 hours post dose.
- For intravenous infusion take samples 4 - 6 hours after start of i.v. infusion, then monitor daily.
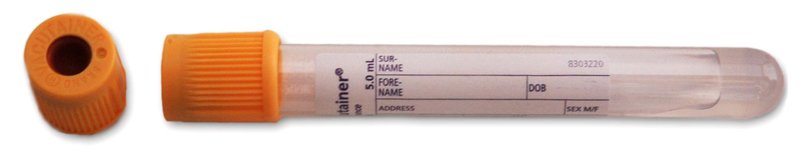
For adults, blood taken into a 5mL gold top gel tube (or rust top for the Acute Unit)
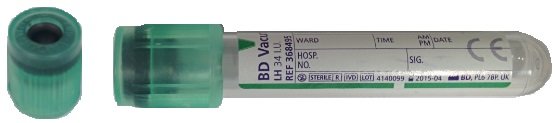
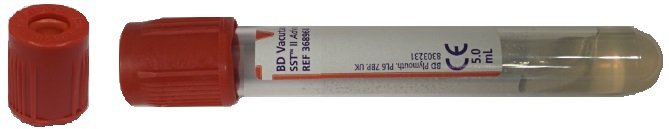
For children, blood taken into a 2mL lithium heparin tube (or a 3.5mL rust top gel tube)
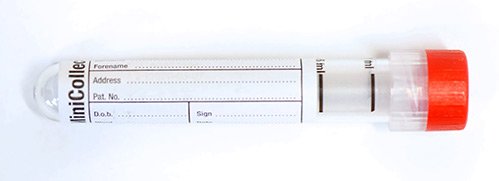
For neonates, blood taken into a 1mL minicollect plain tube or a 0.8mL minicollect lithium heparin tube
Storage/transport
Send at ambient temperature to the laboratory. If unavoidable, samples can be stored refrigerated overnight.
Required information
Relevant clinical details including time relative to dose, prescribed product and route of administration and other medicaton.
Turnaround times
The assays are run throughout the day and night.
The in-lab turnaround time is normally less than 24 hours.
The test can be ordered as an urgent request.
Therapeutic guidelines
| Therapeutic Range | Units | |
|---|---|---|
| Asthma | 10-20 | mg/L |
| Neonatal apnoea | 6-11 | mg/L |
- Side effects are common with theophylline.
- Mild effects such as nausea, headache and jitteriness occur at concentrations below 10mg/L.
- More serious side effects (tremor, agitation, insomnia, diarrhoea, palpitations, cardiac arrhythmias and seizures) occur with increasing frequency at concentrations greater than 20 mg/L (greater than 14mg/L in neonate).
- Serious toxicity is more common with parenteral than with oral administration.
- Rhabdomyolosis and acute renal failure have been described following self-poisoning with theophylline.
- If any symptoms of toxicity despite concentrations within the therapeutic range consider dose reduction.
Further information
To learn more about theophylline visit Lab Tests Online
Page last updated 27/04/2023