Transfusion reaction investigations
The Blood Bank laboratory needs to be informed of any suspected transfusion reaction as soon as possible.
Routine blood tests for Transfusion Reaction investigations;
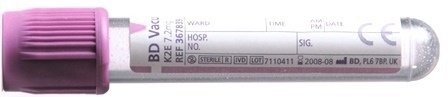
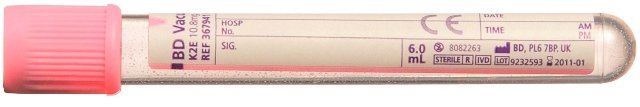
- 6ml EDTA (pink) for repeat cross match and group and screen
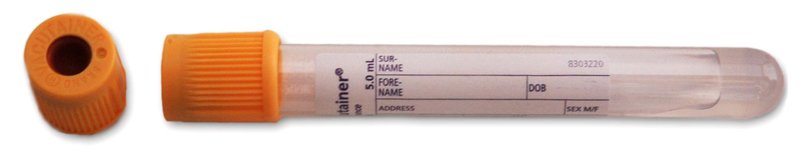
- 6ml clotted sample for U&E’s, LFT’s, LDH, Haptoglobin
- 4ml EDTA (purple) for Full Blood Count
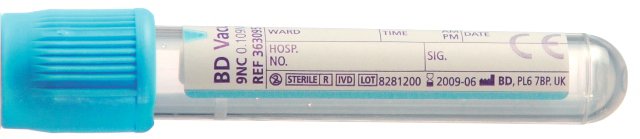
- 2.7ml citrate (blue) for coagulation screen
- Urine sample (to check for haemoglobin / haematuria)
The following factors are known to significantly affect the performance of the examination or the interpretation of the results: lipaemia, sample clotted (if EDTA), haemolysed. Any sample displaying these factors cannot be processed and will be rejected
As well as the above samples, the following needs to be sent to the laboratory:
- Donor pack causing reaction including giving set
- All other units transfused in this episode
- Completed transfusion reaction form (liaise with Blood Bank / Transfusion Practitioner if unable to locate)
- Blood tests as outlined above, including blood cultures if infection is suspected
All reactions considered to be a result of transfusion, except minor allergic or febrile reactions, and without a history of comparable, non-serious reactions, must be investigated with a standard set of laboratory tests together with additional investigations based on the symptoms. The table below summarises the investigations to be completed according to the symptoms presented.
| Symptoms | Investigation |
|---|---|
| Fever (> 2oC rise or ≥ 39 oC), and or chills, rigors, myalgia, nausea or vomiting and/or loin pain | Standard investigations: FBC, Coagulation screen, Renal and liver function tests, G&S for repeat compatibility testing and assessment of urine for Haemoglobin. Specific investigations: DAT, LDH and haptoglobin.Blood cultures from patient |
| Mucosal swelling (angiodema) | Standard investigations: FBC, Coagulation screen Renal and liver function tests, G&S for repeat compatibility testing and assessment of urine for Haemoglobin. Specific investigations: Measure IgA lvel |
| Dyspnoea, wheeze or features of anaphylaxis |
Standard investigations: FBC, Coagulation screen Renal and liver function tests, G&S for repeat compatibility testing and assessment of urine for Haemoglobin. Specific investigations: Check O2 saturation's or blood gases, Chest x-ray If severe or moderate allergy suspected, measure IgA level If severe allergy/anaphylaxis suspected, consider measurement of serial mast cell tryptase (immediate, 3hr, 24hr) |
| Hypotension (isolated fall of ≥ 30mm resulting in level ≤ 80mm) | As for fever. If severe or moderate allergy suspected, measure IgA level. If severe allergy/anaphylaxis suspected, consider measurement of serial mast cell tryptase (immediate, 3hr, 24hr) |
Pulmonary Complications of Transfusion
Transfusion Associated Circulatory Overload (TACO), Transfusion Related Acute Lung Injury (TRALI) and Transfusion Associated Dyspnoea (TAD) contribute significantly to major morbidity after transfusion, and often these are potentially preventable. Early recognition and intervention / treatment is vital. The following video has been created by the SHOT team and provides an overview of pulmonary complications following blood component transfusion.
Watch Pulmonary Complications of Transfusion on YouTube.
Turnaround times
- Preliminary report one working day
- Full report one week
Author: Stuart Lord, Lead Transfusion Practitioner
Reviewed date: 22/04/2025
Next review date: 22/04/2027