Vitamin B12 and Serum Folate
Department of Haematology
Notes
- This test will not be repeated if it has been carried out within the last 3 months.
- This test can be added on to a patient request if the laboratory has an appropriate sample that is less than 3 days old.
- Grossly haemolysed, lipaemic or icteric samples may give erroneous results and will not be processed
- See also: Ferritin Assay; Intrinsic Factor Antibodies
- Tests performed at CGH
Sample Requirements
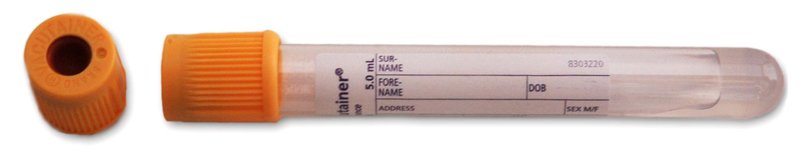
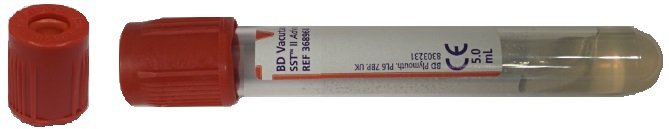
5ml Gold-top SST tube or 3.5ml Rust-top gel tube (Trust users only)
Wherever possible, please send separate samples for haematinics and biochemistry.
Turnaround Times
3 working days from request
Reference Ranges
| Analyte | Range | Units |
| Vitamin B12 | 180 - 914 | ng/L |
| Folate | >4.0 | ug/L |
Please note:
- The reference ranges provided are for adults. Reference ranges for infants and children are dependant on age. Results should be interpreted along with clinical features and other laboratory results.
- B12 levels fall physiologically in pregnancy and this usually does not represent deficiency at a biochemical level. If the mother has otherwise unexplained anaemia (or has other clinical signs of B12 deficiency), consider a treatment trial of B12 replacement as suggested below (following local standard advice for non-pregnant individuals with low serum B12 values). Check intrinsic factor antibody status before B12 treatment. Prescribe parenteral B12 (1mg x 5 over 2 weeks). If intrinsic factor antibody positive, continue 3 monthly parenteral B12 replacement. If intrinsic factor negative withhold further parenteral B12. Repeat blood count and serum B12 estimation after 6 months. If serum B12 low resume 3 monthly B12 replacement. If serum B12 normal, monitor blood count and B12 annually.
Result Interpretation
Serum Folate
Serum folate falls rapidly with an inadequate diet despite sufficient body stores . It is however more reliably analysed than Red Cell folate and is therefore used to screen for folate deficiency.
The common causes of deficiency are inadequate diet, malabsorption, anti-folate drugs (especially anticonvulsants) and occasionally in association with any disease that causes increase cell turnover, e.g. exfoliation.
Vitamin B12
Interpretation is difficult. The following observations are offered.
- In clear cut deficiency, levels of B12 are nearly always <145 ng/l and usually <100 ng/l.
- Pernicious anaemia is the cause of the majority of severe deficiencies in adults. Around 50% of patients with pernicious anaemia have intrinsic factor antibodies while this antibody is rarely seen in normal controls. Parietal cell antibodies are present in 90% of patients but are also seen in 1 - 2% of normal controls.
- Patients with B12 in the borderline range (145 - 180 ng/l) may have either early B12 deficiency or be healthy "low normal".
- Neurological disease or glossitis may occur without anaemia or macrocytosis and may be irreversible.
- Interpretation of early megaloblastic change in the marrow is difficult and cannot be reliably distinguished from myelodysplasia.
The following is advised:
Testing should be restricted to those with a suspected vitamin B12 deficiency (macrocytosis, anaemia, neurological deficit, glossitis or clinical condition known to cause B12 deficiency) and should not be used as a screening test.
When the B12 level is less than 145 ng/l a presumptive diagnosis of B12 deficiency is made. Where the cause is not known, the laboratory will automatically check for intrinsic factor antibodies. If these are negative, a clinical decision has to be made as to whether further investigation is necessary for patient management. If the B12 is between 150 and 180 ng/l, a therapeutic trial should be given. If there is a clinical response then a diagnosis of B12 deficiency is made and the appropriateness of further investigation as to cause should be determined.
If there is no response, it is likely that the patient is not B12 deficient and other causes of the clinical problem must be sought.
If further investigation is required, please contact a Consultant Haematologist.
Updated: October 2025