Central Serous Chorioretinopathy (CSCR)
The information on this page will help to answer some of the questions you may have about the eye condition Central Serous Chorioretinopathy, commonly called CSCR.
On this page
-
What is CSCR?
-
What are the symptoms of CSCR?
-
Who might develop CSCR?
-
What are the causes of CSCR?
-
How long will I have CSCR?
-
How is CSCR diagnosed?
-
How do you treat CSCR?
-
Treatment options
-
Medication
-
Will glasses help?
-
Coping with CSCR
-
Contact information
-
Further information
-
Sources of information used for this page
What is CSCR?
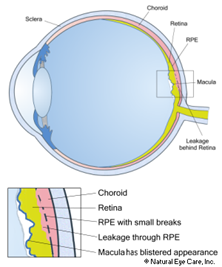
CSCR is a condition that affects the retina. This is the light sensitive layer at the back of your eye which captures images and enables you to see. The macula is the part of your retina responsible for your central vision. Special cells called retinal pigment epithelial cells (or RPE cells) have a pump action that helps to nourish the retina. The blood vessel layer beneath the retina is known as the choroid.
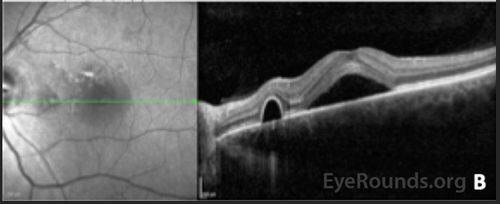
Any abnormality to the function of the RPE cells or the choroid can lead to a build-up of fluid between the layers of the retina. If the fluid affects the macula, you may experience painless blurring of your central vision.
What are the symptoms of CSCR?
Symptoms can include:
- A fairly sudden onset of blurry vision in one eye.
- A blurry, dim blind spot in the centre of your vision.
- Objects appearing in miniature with the affected eye.
- Distortion of straight lines.
- Colours appearing ‘washed out’.
Who might develop CSCR?
This condition is 6 times more common in men than women, and most often affects people aged between 20 and 50 years old.
What are the causes of CSCR?
In most cases there are no specific causes that can be found to explain why CSCR has occurred. However, researchers have identified several risk factors as the condition occurs more frequently in people:
- who experience high levels of stress, both physical and emotional.
- who use some stimulant drugs such as amphetamines, smoking and caffeine.
- with ‘Type A’ personalities (competitive, highly organised, ambitious, hard to relax).
- who use steroids, sometimes known as corticosteroids. Steroids are prescribed in various forms for a number of common conditions including inhalers for asthma, skin cream for eczema and tablets such as prednisolone for inflammatory conditions.
- with Cushing Syndrome (an over production of the body’s steroid hormone - cortisol).
- with high blood pressure.
- with obstructive sleep apnoea.
How long will I have CSCR?
Generally speaking, CSCR can be grouped into 3 categories, by the way it progresses:
- Most people will recover within 3 to 6 months without any need for treatment. Vision often returns to how it was before CSCR developed. Between 30 to 50% of people will experience a further episode of CSCR in either the same or other eye.
- CSCR which lasts up to 12 months may require treatment. Your vision may be slightly more at risk because the retinal layers can become damaged from prolonged swelling.
- CSCR which lasts over 12 months is very rare. This can lead to further changes such as retinal pigment epithelial detachment (RPE) or bullous retinal detachment, where fluid collects under the retina, away from the macula. Long-term CSCR can lead to loss of function of RPE cells resulting in a permanent worsening of vision.
A few eyes with CSCR can develop abnormal blood vessels (macular neovascularisation) needing additional treatments with intravitreal anti-VEGF therapy.
Anti-VEGF treatment is given as an injection into the white of your eye (the sclera). The drug is injected directly into the vitreous, the jelly that fills your eye. This is called an ‘intravitreal’ injection. The procedure is generally very straightforward and quick and is not usually painful.
How is CSCR diagnosed?
CSCR is diagnosed following an examination by your eye doctor. When you come to the eye clinic you will have your vison checked, so it is important to bring your glasses with you.
Eye drops will be used to enlarge your pupils in order that the eye doctor can examine your retina. The eye drops will make your vision blurred for between 4 and 6 hours. It would not be safe for you to drive during this time so you should arrange transport home where necessary.
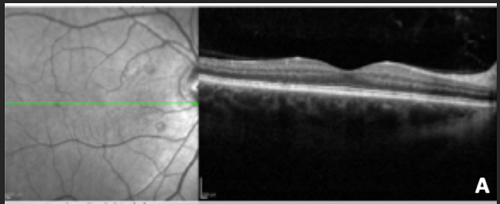
A scan called an OCT scan will be performed to look at the different layers of the retina in detail. This is a quick and painless procedure.
Occasionally a dye test will be requested in order to examine the blood vessels in the retina. This test involves an injection of dye through a small plastic tube into a vein in your arm (a cannula). This test would take place at a separate clinic appointment and would be explained in more detail at the time.
When these tests are completed, your ophthalmologist will discuss the results, available treatment options and how to manage any risk factors you may have.
How do you treat CSCR?
Observation
In the majority of cases, the condition settles down on its own, within 6 months, and no treatment is necessary. Any triggers such as corticosteroid use may be reviewed and stopped if advised by your doctor.
Lifestyle changes
After an episode of CSCR, you may wish to see your GP to discuss control of any possible risk factors such as counselling for stress management, ways of improving sleeping patterns, smoking cessation and reducing alcohol and caffeine consumption.
Some patients may experience a recurrence of their condition leading to worsening of their vision. In these cases, treatment may need to be considered.
Currently there is no treatment that is approved by NICE (National Institute for Health and Care Excellence). Research trials are being carried out to discover new types of treatment.
Treatment options
Photodynamic Therapy (PDT)
This is a form of ‘cold laser’ treatment, using a non-toxic light sensitive dye which is injected into a vein in your arm.
The dye molecules are triggered by infrared light from the laser, converting into a substance that destroys the abnormal blood vessels without damaging the surrounding tissue.
The aim of the treatment is to slow down or stop the development of abnormal blood vessels at the macula and leakage of fluid in the retina. This results in removing the retinal fluid in about 80% of eyes with 1 to 2 treatment sessions, with a reduction in symptoms of distortion and improvement of vision. However, it has also been found that not all patients get their vision back, despite the retinal fluid being removed.
This procedure does carry some risks (estimated 1% risk of vision loss) and not everyone is suitable for the treatment. This treatment would be carried out at an outpatient appointment.
Thermal laser
Your ophthalmologist will apply the laser to the vessels in your retina which are leaking. This treatment is useful if there is a leakage spot which is not involving the central macula. It cannot be used if the leakage occurs in the fovea (which is the very central area of your macula) as the laser can leave a scar and this could permanently affect your vision.
Micropulse laser
Unlike traditional thermal laser, micropulse lasers use very low power treatment with no visible retinal changes and therefore do not cause scarring. This means that treatment can be given to areas in central macula. Studies have shown that this treatment has a much lower success rates than PDT laser treatment.
Medication
There are currently no licensed medicines that have been shown to be effective for treating CSCR. Drugs which block steroids effects such as elenerone have been used off licence with initial reports of improvement.
An off-licence medicine is one that is not licenced for the treatment of your condition (CSCR), but it will have a licence to treat another condition and has undergone clinical trials for this.
Your doctor may recommend using eplenerone if they think it will treat your condition effectively and the benefits are greater than any risks.
Will glasses help?
Getting new glasses will not help to improve your vision with CSCR. The prescription will change depending on how much fluid is beneath the retina and only help temporarily. It would be advisable for you to wait until the fluid resolves completely before updating your current glasses or getting new ones.
Coping with CSCR
How much the CSCR will affect your vision varies from person to person. Most people do not notice any difference unless they cover the eye which is not affected. However, some people may be aware of the change all of the time and have difficulty with their 3D vision, for example judging distances, misjudging steps and the position of objects. This could become less of a problem over a few months as the brain adjusts to a new level of vision, making the eye which sees better the ‘dominant’ eye.
If the affected eye was your good eye and you have a sight problem in your other eye, then you may need to make changes or use aids to make the most of your remaining sight. This may mean making things bigger, using brighter lighting or using colour to make things easier to see. A low vision assessment in the hospital eye clinic can be arranged and a specialist optometrist can explore these things with you.
Contact information
If you would like to speak to someone regarding concerns you may have about life at home, work, education or emotional issues relating to your eye condition, please contact our Eye Clinic Liaison Officers (ECLO) who will be happy to offer support and guidance. Their details are:
Louise Birt
Tel: 07702 961060
Email: Louise.Birt@RNIB.org.uk
Gary Learmonth
Tel: 07925 034799
Email: gary.learmonth@rnib.org.uk
If you have any emergency concerns regarding your eye condition, contact the Ophthalmology triage line to speak to a specialist nurse.
Ophthalmology Triage
Tel: 0300 422 3578
Monday to Friday, 8:00am to 1:00pm and 2:00pm to 5.30pm
Saturday 8.00am to 1.00pm
Out of hours calls will be diverted to the eye doctor on call.
Further information
Royal National Institute of Blind People (RNIB)
This is a charity offering information about many different eye conditions. RNIB can also provide information in large print or in audio formats.
Tel: 0303 123 9999 (Helpline)
Email: helpline@rnib.org.uk
Website: www.rnib.org.uk
Insight Gloucestershire
This is a local independent countywide charity that supports people living with sight impairment.
Tel: 01242 221 170
Monday to Friday, 9:00am to 1:00pm
Email: enquiries@insight-glos.org.uk
Website: www.insight-glos.org.uk
Macular Society
PO Box 1870, Andover SP10 9AD
Tel: 0300 3030 111
Sources of information used for this page
Royal National Institute of Blind People
Available at: https://www.rnib.org.uk/eye-health/eye-conditions/central-serous-retinopathy Accessed 24th August 2024
East Sussex Healthcare NHS Trust - Patient Information ‘CSR’
Available at: https://www.esht.nhs.uk/wp-content/uploads/2019/08/0753.pdf Accessed 24th August 2024
Moorfields Eye Hospital NHS Foundation Trust - Patient Information ‘CSCR’
Available at: https://www.readkong.com/page/central-serous-chorio-retinopathy-cscr-moorfields-eye-4367206 Accessed 24th August 2024
Oxford University Hospitals NHS Foundation Trust. Central Serous Chorioretinopathy. Information for parents and carers.
Available at: https://www.ouh.nhs.uk/patient-guide/leaflets/files/94025chorioretinopathy.pdf Accessed 28th August 2024