Information about day case ERCP (Endoscopic Retrograde Cholangio-Pancreatography)
You have been advised to have an ERCP either to help us find out the cause of your symptoms or for the management of your symptoms. This page should help answer any questions you may have.
It is important to understand that this procedure is performed using throat anaesthetic, sedatives and analgesia.
ERCP is likely to include therapy (treatment). If you currently take anticoagulant medication (blood thinners) or medication for diabetes, you will be given advice about when to stop them before the procedure. If you do not receive advice at your pre-assessment appointment or you have further questions, please contact the Medication Advice Line. Failure to follow the advice given may result in the ERCP not going ahead.
It is important that you understand the procedure and associated risks before having the ERCP. Therefore, it is essential that you read the information given in this leaflet.
For the ERCP to take place the following must be in place:
- You must have someone to take you home and stay with you for 24 hours after the ERCP.
- You have stopped your anticoagulation and diabetes medication as discussed with the department/pre-assessment nurse.
- You have signed the consent form.
What is an ERCP?
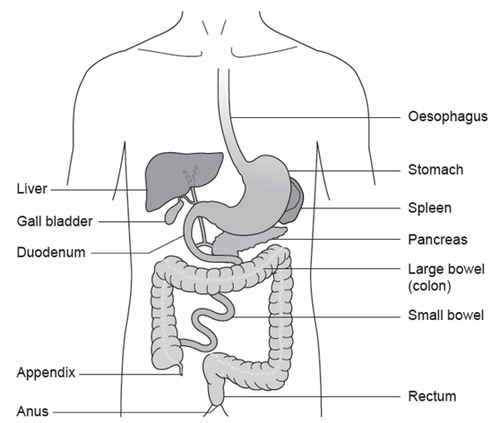
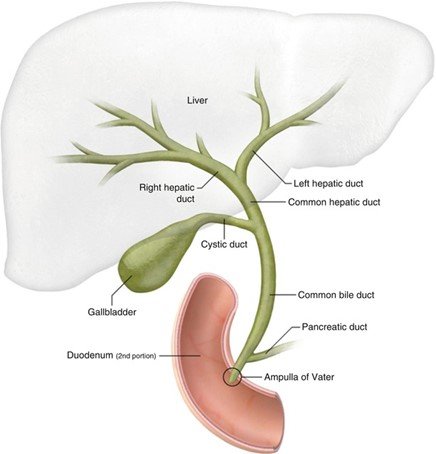
An ERCP is an examination, using a camera, of the biliary and pancreatic tubes (ducts). A telescope (also known as a scope) is passed through your mouth, down your oesophagus, into your stomach and around the first bend of the small intestine (duodenum) to the opening of the ducts (ampulla). The scope that is used is a long flexible tube which is thinner than your index finger and has a tiny camera at the end.
X-rays are carried out at the same time as the camera procedure. Dye is injected into the ducts of the biliary and pancreatic systems while the X-ray is taken. This will show any problems related to these systems.
Therapies (treatments) that may be carried out during the procedure
Sphincterotomy
This is a cut made into the bottom of the bile duct to help pass a stone, widen a narrowed duct, or insert a plastic tube (stent).
Balloon clearance
If a stone or sludge can be seen in the biliary ducts, a catheter with a deflated balloon can be passed up the duct and then inflated. This is then gently pulled down the duct, removing the stone and sludge.
Basket clearance
An instrument can be passed up the duct and then used to grasp the stone and bring it out.
Stent insertion
If there is a narrowing or if a stone cannot be removed, then a plastic or metal mesh tube the size of a biro refill can be put into the bile duct to allow bile to drain and to relieve any jaundice (yellow discolouration of your skin as a result of bilirubin entering the blood stream). This mesh tube may need to be taken out or replaced with a new one after a period of time. This will be discussed with you before you are discharged.
Biopsy
A small piece of tissue (a biopsy) may be taken from the lining of your duodenum for further examination in a laboratory. This is not painful and is carried out by using tiny biopsy forceps through the telescope.
Possible risks of ERCP
It is important that you fully understand the procedure and the risks related to it. We want to give you as much information as possible about ERCP treatment so that you can make an informed decision. This procedure is successful in 85 to 90 out of every 100 cases, but in difficult cases it may need to be repeated. The risks of having ERCP are small, less than 3 in 100 cases overall. These risks will be discussed with you at the pre-admission clinic or before your procedure.
Sedation
Sedation is used to make you sleepy during the procedure. The main complication from sedation is that it can affect your breathing. The risk of this happening is very low because you will be carefully monitored throughout and given extra oxygen during the procedure.
Bleeding
This can happen if you have a sphincterotomy. The risk of this happening is 1 in every 100 cases.
Perforation
This is a tear or hole in the wall of the duodenum or bile duct. It can happen when therapy is undertaken. The risk is about 1 in every 500 cases.
Pancreatitis
This is inflammation of the pancreas which is a serious condition that will mean you would need to stay in hospital and be carefully monitored. The risk of this complication is 3 to 5 in every 100 cases. In 1 in every 100 cases, severe pancreatitis can be life-threatening.
Ascending cholangitis
This is infection within the bile duct and is more likely if the duct is blocked.
ERCP is generally a safe procedure. The risks we have listed can usually be managed with medical treatments, but sometimes surgery may be necessary. You will be able to ask any questions you may have at the Pre-admission Clinic and before the procedure takes place.
Alternative procedures
A different procedure called a Percutaneous Transhepatic Cholangiography (PTC) can be carried out. Your specialist will talk to you about this if they think it is suitable for you.
During a PTC a needle is passed through the skin and muscle into the liver and then into the bile ducts from above. It is more invasive than an ERCP but may sometimes be needed because of your condition.
An operation may be necessary to remove your gallbladder (called a cholecystectomy) and any gallstones at the same time. You can talk about these alternatives with your specialist.
Pre-assessment Clinic
You may be pre-assessed ahead of your ERCP procedure. This will be done by a specialist nurse either by telephone or in clinic.
You will be asked a series of questions regarding your medical history and any medicines you are currently taking. The nurse will also want to know if you have any allergies or have had any bad reactions to any medicines.
The procedure will be explained in detail to you during this appointment along with any risks so that you fully understand.
You may need a blood test prior to your procedure. The specialist nurse will arrange this with you if necessary.
Admission to hospital
You will be given a date for when you need to come into hospital for your procedure.
To allow a clear view during the procedure, your stomach must be empty. You must not have anything to eat for 6 hours before your appointment time. You may drink water up to 2 hours before your appointment time. Please do not suck sweets or chew gum as this could stop your procedure going ahead.
For this procedure you will be asked to take off your clothes and put on a hospital gown.
You will have a small tube (cannula) inserted into a vein in the back of your hand. This is for the doctor to give you any medication needed.
You will be asked to sign a consent form if you have not already signed it in clinic.
The procedure
A nurse will go with you to the endoscopy room where your ERCP will take place. A nurse will stay with you during the procedure.
In the endoscopy room, you will be asked to take out any dentures you are wearing.
A local anaesthetic spray will be sprayed into your throat to numb it.
You will then be made comfortable on a couch lying on your front with your head to one side. You will be linked to a heart monitor so that we can record your oxygen levels and blood pressure during the procedure. A small tube will be placed into your nostril to give you oxygen while you are having the procedure. The doctor will then give you sedation through the cannula.
You will also be given medication in the form of a suppository placed in the rectum (back passage) called diclofenac (Voltarol®). This is given to reduce the risk of pancreatitis.
To protect your teeth and the scope, a plastic mouth guard will be put between your teeth or gums (if dentures have been removed). The endoscopy tube will then be gently pushed through the mouth guard. When it reaches the back of your throat, you may be asked to swallow to help the tube go down. This will not affect your breathing. Some air will be passed through the scope to gently inflate the duodenum and allow a clearer view.
You may feel wind-like discomfort and belch some air up during the procedure, but please do not be embarrassed as this is normal. Any saliva in your mouth will be taken away by the nurse caring for you using a small suction tube. When the scope is taken out, most of the air we put into your stomach will also be taken out.
After the procedure
After the ERCP is over, the nurse caring for you during your procedure will take you to the recovery area. You may be asleep or drowsy during this time. Recovery nurses will keep checking your breathing, pulse and blood pressure while you recover.
You may feel a little bloated or have some discomfort in your stomach after the test.
Your throat will still feel a little numb from the throat spray, but this will slowly wear off. Your throat may then feel a little sore, which could last for the rest of the day.
You will be allowed to drink and eat after the procedure. If you feel unwell or have any pain after the procedure, please let the nursing staff know.
Going home
Most people will be discharged the same day as the procedure, but you will be asked to remain in the department for 4 hours after you have had something to eat.
Before discharge you will be given information about the outcome of the ERCP and any further tests which may be necessary. You cannot drive yourself home or travel home alone after having sedation. You will also need to arrange for somebody to be with you overnight.
You must not drive for 24 hours after having sedation.
You will receive a copy of the ERCP report that is sent to your GP.
Contact information
ERCP Advice Line (answer machine)
If you have any questions relating to your ERCP procedure, please leave a message. The ERCP Specialist Nurse will return your call normally within 24 hours, Monday to Friday only.
CHECK
If you have not received a call back within 24 hours, please contact the Medication Advice Line at the relevant Endoscopy Unit)
Tel: 0300 422 2314
Monday to Friday, 8:00am to 6:00pm
You can also contact the Endoscopy Unit via the hospital switchboard.
Gloucestershire Hospitals Switchboard
Tel: 0300 433 2222
When prompted, ask for the operator then ask to be put through to your consultant’s secretary.
Medication Advice Line (answer machine)
If you have any questions relating to your medication, please leave a message. A member of staff will return your call normally within 24 hours, Monday to Friday only.
Cheltenham General Hospital
Tel: 0300 422 3370
Monday to Friday, 8:00am to 6:00pm
Gloucestershire Royal Hospital
Tel: 0300 422 8232
Monday to Friday, 8:00am to 6:00pm
Saturday and Sunday, 9:00am to12:00 midday