My Catheter Passport
Please take the attached booklet, below with you to all healthcare appointments and hospital admissions. You should also keep it with you when travelling. This passport will help you to understand what a catheter is, why you may need one inserted, and how you should look after it. It also has space for healthcare professionals to record important information about your catheter, and for you both to record decisions that you’ve made together about your care.
On this page
-
Contact us
-
Your important contact numbers
-
Why do I need a urinary catheter?
-
Alternatives to an indwelling catheter could be:
-
How does the urine system work?
-
What is a urinary catheter?
-
Your catheter will be attached either to a catheter valve or a leg bag.
-
Catheter valves
-
How do you use a catheter valve?
-
How do I wear the catheter valve?
-
How often should the catheter valve be changed?
-
Leg bags
-
How do I empty the drainage bag?
-
How often should the leg bag be changed?
-
How should the drainage bags be disposed of?
-
What happens at night?
-
When will my catheter need changing?
-
Does a supra-pubic catheter need special care?
-
Going on holiday
-
Storing your catheter supplies
-
Daily catheter care
-
Personal hygiene
-
Frequently asked questions
-
Are there any risks with having a catheter?
Contact us
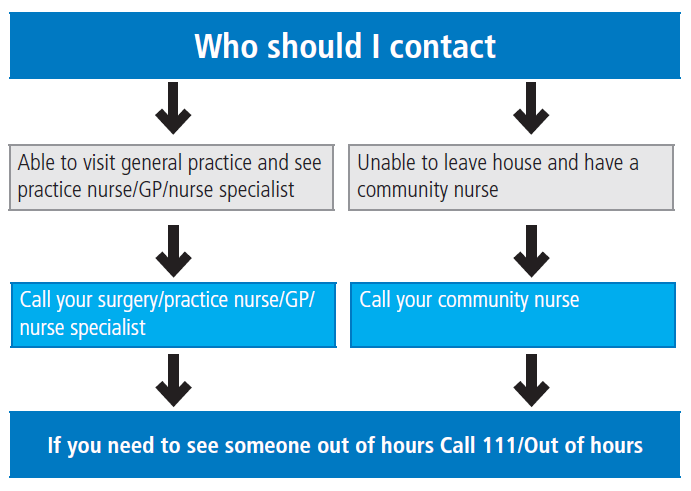
If you have any questions or concerns about your catheter, please contact the appropriate healthcare professional.
Your important contact numbers
Within the booklet below, you may find it useful to write down your important contact numbers, such as; Practice nurse community nurse, Clinical nurse specialist, GP, Hospital team, Bladder and bowel health.
Make sure you keep this record of your catheter and have it with you whenever you have your catheter changed, so your lead healthcare professional (this could be your community nurse/practice nurse/other healthcare professional) can update your catheter details.
Why do I need a urinary catheter?
Many people need to be catheterised at some stage in their lives for many reasons, including:
- to let urine drain if you have an obstruction in the tube that carries it out of the bladder
- to allow you to urinate if you have bladder weakness or nerve damage that affects your ability to pass urine
- to drain your bladder before, during and/or after some types of surgery.
Alternatives to an indwelling catheter could be:
- Intermittent catheterisation (carried out by self or carers)
- Containment products (pads)
- Urinary sheaths (male patients only)
How does the urine system work?
The kidneys filter waste products from the blood to produce urine. Urine enters the bladder via 2 tubes called ureters. When the bladder is full, urine is passed out of the body through the urethra. If the bladder does not work properly or needs to be rested after an operation, a urinary catheter will be inserted to keep the bladder empty. If the bladder is not emptied regularly, and urine stagnates, this can be a risk factor for infection.
What is a urinary catheter?
A catheter is a hollow flexible tube, which drains urine from your bladder. The catheter reaches the bladder either by passing through the urethra, or through a channel made in the abdominal wall, just above the pubic bone. This is called a supra-pubic catheterisation. Once the catheter is in place, a small balloon at the catheter tip is inflated with sterile water. This prevents the catheter from falling out. As urine enters the bladder from the kidneys, it continues to drain down the catheter into a drainage bag. With a catheter in place, you should not need to pass urine in the usual way.
Please see the images for Male & Female Urethral and Subrapubic catheters within the PDF booklet, below.
Your catheter will be attached either to a catheter valve or a leg bag.
With a catheter valve, your urine collects in your bladder, which can be emptied at regular intervals by releasing the valve tap.
A leg bag is a simple drainage bag to collect your urine. This is strapped to your leg. If you are bed bound, it may be a belly bag or a two litre bag rather than a leg bag. You should avoid the leg bag getting heavy. Empty the leg bag before it’s completely full, around half to two-thirds full. See over for more information.
Catheter valves
The catheter valve is a tap-like device, which fits on to the end of the catheter tube (urethral or supra-pubic). The valve can be used whether the catheter is a temporary or permanent arrangement. The bladder is now able to store urine and can be emptied intermittently by releasing the tap on the valve, thus helping to maintain the normal function of the bladder.
The catheter valve is more comfortable and discreet compared to a leg bag. It may also reduce the risk of infections and blockages as it allows intermittent flushing of the catheter with urine when you drain the bladder.
If the catheter is to be used for a short period of time, a catheter valve will help maintain the bladder’s capacity.
How do you use a catheter valve?
The catheter valve should be opened to drain urine when the bladder feels comfortably full or approximately every 4 hours. The aim is to empty a volume around 350mls to 500mls, an average bladder capacity. If the volume of urine drained is below 200mls, reduce the number of times the valve is opened to encourage a larger bladder volume to be emptied. If the volume that is drained is over 500mls then increase the amount of times in the day the bladder is emptied. Urine drainage via the valve can be emptied directly into the toilet or suitable container.You should open the valve to empty your bladder before opening your bowels.
Should you experience discomfort or any leakage down the sides of the catheter, try draining the urine more often.
To help prevent infection, only disconnect the valve weekly when it is replaced with a new one.
How do I wear the catheter valve?
The catheter valve will tuck nicely into your underwear; alternatively the valve can be supported on to the upper thigh with a catheter fixation strap which can be supplied by the nurse managing your catheter care.
The catheter valve can also be used with a bed bag at night or with a leg bag during the day if toilet access is likely to be a problem.
How often should the catheter valve be changed?
The catheter valve should be changed every 5 to 7 days or earlier if it is damaged. You should seek advice, support and training by a health care professional, before you attempt to change the catheter valve. If this procedure is not performed correctly, then it could increase the risk of an infection.
Always wash your hands (see page 16 for hand washing technique) before handling the catheter valve. Drain the bladder first, then remove the old catheter valve and replace it immediately with a new one. Avoid handling the section of the valve which is inserted into the catheter to prevent introduction of an infection. Place the old catheter valve into a plastic bag before disposing of it into the household rubbish. Wash your hands again after changing the valve.
Leg bags
Securing your catheter and leg bag
Ensure you use a catheter fixation device. These devices are used to fix the catheter to your thigh to hold the catheter securely. The devices should be used to reduce the risk of catheter/urine infections and prevent the catheter from being pulled, which could cause you urethral trauma. Common forms of fixation devices are adhesive clips or Velcro straps or catheter sleeve. All indwelling catheters should have a fixation method. If you do not have a fixation device attached to your catheter, please speak to the healthcare professional managing your care, who will advise you on the appropriate fixation device for you.

When attaching the leg bag using the straps provided, always ensure they are placed through the slots and behind the inlet tube rather than over as this can block the tube.
The choice and size of the bag and the length of tubing depend on where you want to wear it and how much urine you pass. When wearing trousers, a long tube bag may be more convenient as it is possible to roll up the bottom of the trouser leg and access the tap at the base of the bag for emptying urine. Short tube leg bags can be worn on the thigh and are discreet under skirts, shorts and dresses. Men should try to change the position of the leg bag frequently to avoid damage to the penis from the catheter rubbing in one position.
As the leg bag fills, it becomes heavy. Do not allow the bag to become too full.
How do I empty the drainage bag?
- You should empty the leg bag before it’s completely full, around half to two-thirds full of urine.
- Wash your hands thoroughly
- Open the tap at the bottom of the bag and drain the bag into a toilet or suitable container
- Close the tap after you have drained the bag
- Wash your hands again.
- To help prevent infection, only disconnect the leg bag when it is replaced with a new one.
- It’s important you or your carers learn to manage your leg bag. If you can not manage you will need to consider a package of care to support this.
How often should the leg bag be changed?
Most leg bags are changed on a weekly basis (but sooner if damaged); it is best to change your leg bag on the same day of the week. Empty the attached leg bag before changing to your new one.
- Wash your hands before and after.
- Open the new leg bag, but don’t remove the protective cap.
- Remove the attached leg bag carefully. Don’t pull or use excessive force.
- Point the end of the catheter upwards as you detach the leg bag to prevent leakage. Dispose of old leg bag into a plastic bag (follow your local council’s policy for disposal).
- Carefully remove the protective cap from the new leg bag. Do not touch the nozzle once you have removed the cap.
- Gently insert the new leg bag connector to the catheter. Take care not to touch the plastic nozzle.
How should the drainage bags be disposed of?
Both the leg and bed bags should be emptied and placed into a plastic bag before disposing of it into the household rubbish.
What happens at night?
- A bed bag or overnight bag - This is used at night. The bed bag is larger than the leg bag and is connected to the bottom of the leg bag or valve to collect the urine, which drains from the bladder overnight. This is known as the link system.
Remember, you must open the leg bag valve or catheter valve to allow drainage and when the bed bag needs to be removed, close the valves to prevent any accidental leakages.
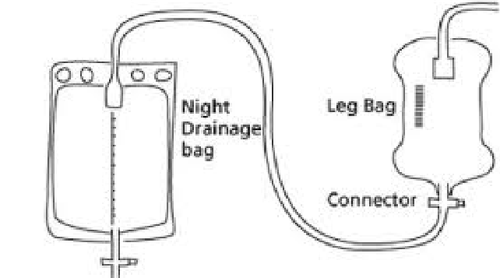
Decontaminate hands using soap and water following these 6 steps. If using soap wet hands first. Visibly clean hands may be decontaminated using alcohol hand rub following these 6 steps. At night, connect the bed bag to the bottom of the leg bag and open the tap of the leg bag to allow urine to drain freely into the bed bag. Support the bed bag on a stand, which should be supplied with your catheter supplies, or hanger and always keep the bed bag down lower than your bladder, because urine cannot drain up hill. Do not allow the bed bag to lie directly on the floor. Remember to check that the bed bag tap is closed. The following morning, close the tap on the leg bag and remove the bed bag.
If you are a patient in a hospital or a communal living environment, the bed bag should be only used once and thrown away in a clinical waste bin.
In shared living circumstances (such as care homes, shared housing, hostels etc) the risk of infection increases, so the bag should be single use, and disposed of after each night.
If your bag is re-usable: In the morning, disconnect the night bag, empty it, wash through with soapy water and store it in a clean place until you reconnect it. This bag should also be changed according to the manufacturer’s instructions.
When will my catheter need changing?
Your healthcare professional will advise you on how often your catheter needs changing and how to obtain further supplies of catheter equipment. It is always important to keep spare equipment in your home.
Does a supra-pubic catheter need special care?
The usual advice for caring for any catheter also applies to a supra-pubic catheter. The area around the insertion site should be washed with plain soap and water daily. Again, avoid using any creams or talcum powder around the entry site keeping the area dry and free of a dressing.
Going on holiday
If you are going on holiday make sure that you have a spare catheter and plenty of catheter valves and/or drainage bags to take with you. Pack these in your bag for the plane as well as in your suitcase, in case your suitcase gets lost.
Collect your supplies from where ever you normally get your prescription from or speak to your healthcare professional about arranging a delivery to your home address by a delivery appliance company.
Storing your catheter supplies
Store the catheters, catheter valves or drainage bags in their original packaging. Keep them in a dry safe place away from direct heat and sunlight.
Always keep a spare catheter at home in case of an emergency.
Daily catheter care
Hand washing techniques before and after touching your catheter
Decontaminate hands using soap and water following these 6 steps. If using soap wet hands first. Visibly clean hands may be decontaminated using alcohol hand rub following these 6 steps.
Each step consists of 5 strokes rubbing backwards and forwards.
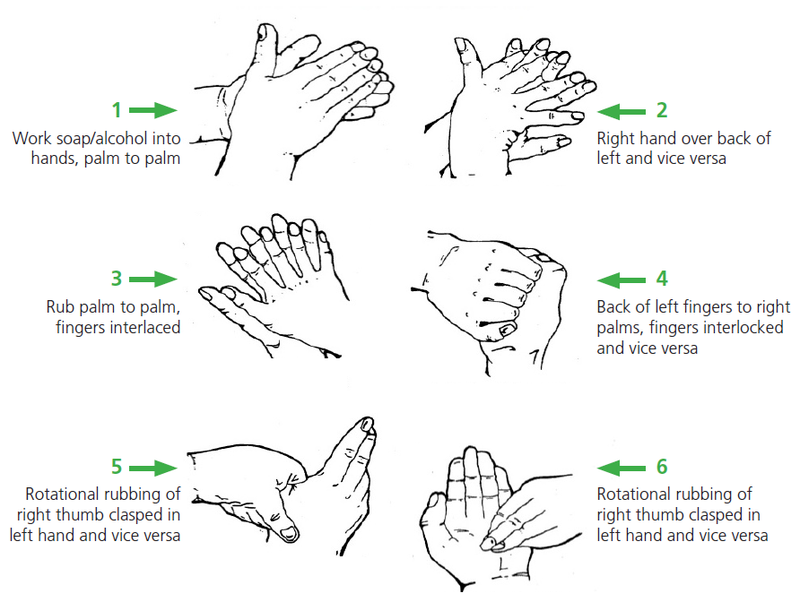
If using soap and water rinse hands under running water and dry thoroughly. If using alcohol get use above technique until alcohol has evaporated.
Personal hygiene
Washing
- Wash your hands with soap and water before and after touching your catheter using the method above.
- If possible, have a daily shower (preferably) or bath. Do this with your leg bag or valve attached.
- Wash the skin in the area where the catheter enters the body with unperfumed or mild soap and water at least daily and after using the toilet if possible. Use a clean flannel or cloth for this purpose only.
- Wash around the catheter tubing, moving in a direction away from the body.
- Avoid using talcum powder or ointment or creams around the catheter.
If you have a urethral catheter:
- Men should be careful to wash under their foreskin, replacing afterwards, unless you have been circumcised.
- Women should always wash the genitals from front to back, to avoid moving faeces from your bottom to the catheter.
If you have a suprapubic catheter:
- Some people may experience a slight discharge from around the catheter site. If this happens then contact your healthcare professional who will tell you the best way to treat it.
- Avoid pulling or restricting your catheter by wearing loose comfortable clothing. Tight clothing can cut off the flow of urine and cause skin irritations.
Diet and fluid intake
People with catheters need to take care to keep their bladders and bowels healthy. It is important to avoid constipation. Constipation can cause obstruction of the catheter, and drainage problems can occur. It is recommended that you follow a healthy diet, including eating 5 fruit or vegetable portions daily, as recommended by the Department of Health. Do not strain on the toilet. Relax and allow yourself enough time and privacy to empty your bowels fully.
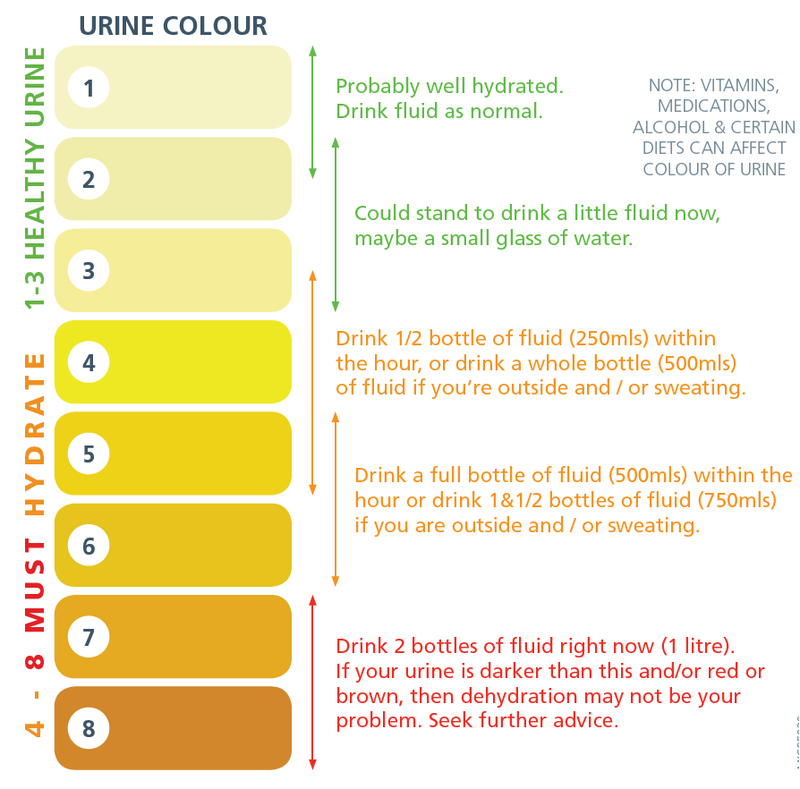
Drinking approximately 8 cups or 2 litres of fluid daily, is strongly recommended to ensure the catheter drains well and helps keep the urine clear. If your urine is orange/dark brown, you may not be drinking enough fluid. However, some medication and foods can discolour urine. Your nurse will be able to discuss this with you.
Drinking alcohol will not affect your catheter. However, if you are taking certain medicines or recovering from surgery, your doctor may advise against drinking alcohol. This depends on your individual circumstances. Please ask your healthcare professional if you are uncertain.
Dehydration Urine Colour Chart
The following Dehydration Urine Colour Chart will help you use your urine colour as an indicator of your level of dehydration and what actions you need to take to help return your body back to a normal level of hydration.
For more information visit www.urinecolours.com
Frequently asked questions
Can I work and exercise as normal?
You can return to work, exercise or go on holiday as soon as you feel able to and your doctor has said you are fit enough to do so.
Can I have sex with an indwelling urethral catheter in place?
Intercourse is usually possible with a urethral catheter for both men and women.
Men can tape the catheter along the shaft of the penis and secure it in place with a condom.
Women can tape the catheter up onto the abdomen.
The drainage bag should always be emptied before sexual activity and both partners should wash their genital area thoroughly before and after intercourse. It helps to use plenty of water- based lubrication, such as K-Y® jelly (but not Vaseline®).
A supra-pubic catheter may make sexual intercourse easier.
Troubleshooting
If you are worried about your urine, or that your catheter is leaking/not draining, here are some checks.
- Are your food and fluid intake adequate?
- Are you eating a healthy, diet?
- Are you constipated? If you are already following the previous tips seek medical advice.
- Is the drainage bag below the level of the bladder, particularly when sitting in a low or reclining chair?
- Is the tubing twisted, or restricted by tight clothing?
- Is the tubing extended or pulled tight towards the bag?
- Is the catheter tube connected to the drainage bag correctly?
- Are the leg straps stopping urine flowing into the bag?
- Is the bag too full? If in doubt empty the bag.
- Change your position and walk around if you are able and it is safe.
- If your catheter is leaking but still draining some urine, this may be due to bladder spasms—where the bladder contracts as a result of irritation from the catheter. Bladder spasm can make you feel like you need to pass urine or you may experience abdominal cramps. This usually stops and is nothing to worry about. If the problem persists, contact your health care professional for advice. Sometimes patients who have bladder spasms can be treated with medication.
- If your catheter is not draining, you need to contact your health care professional.
If your catheter is painful:
- Check that your catheter and drainage system are adequately secured
- Check that the catheter and tubing is not kinked or that you are not sitting on the tubing
- For men, check that the foreskin is in the correct position and not swollen
- Observe for any redness, inflammation or pus or discharge at entry site
- Inform your GP or nurse of any pain experienced with your catheter.
If you have any questions please speak to the nurse managing your catheter care.
When to call for help
Help should be sought if any of the following occurs:
- your catheter is draining little/no urine despite adequate fluid intake and following the troubleshooting guide (on page 20)
- there is no urine in the bag after 4 to 5 hours, or you start experiencing bladder discomfort
- you feel warm, flushed or shivery, as you may have an infection
- your urine has a strong smell, is dark in colour or becomes thick and/or cloudy and does not improve with taking more fluid (if able or advised)
- you experience lower stomach or back pain
- you have increased stomach swelling with no other cause
- there is bright red blood in your urine
- the catheter entry site becomes red and sore
- you have bleeding into or around the catheter
- you have enough urine leaking around the catheter to make your clothing wet and you have already followed these self-help measures
- your catheter falls out.
Are there any risks with having a catheter?
What are the risks of having an indwelling urinary catheter?
An infection can occur within a few days of catheterisation often with-out any symptoms and bacterial levels increase as long as the catheter remains in place.
How will I know if I have a UTI?
Having a catheter in your urinary tract significantly increases your chances of getting a UTI, which is why it is so important to care for it following the advice in this passport.
Signs and symptoms associated with a UTI:
- feeling unwell
- fever with or without uncontrollable shaking
- new pain at lower tummy or back
- becoming agitated or newly confused
- pain around the area where the catheter is put in and/or pus like discharge in the urine
- unusual tiredness
- Nausea and headache
If you have any of the above signs or symptoms, please contact your healthcare professional.
If you are prescribed antibiotics for a UTI:
You should make sure you are drinking plenty of fluids (2L/8cups) and make contact with your healthcare professional.
- Make sure you follow the instructions given with the antibiotic and finish the course.
- Using antibiotics only when we need to helps reduce the chances of bugs causing the infection becoming resistant to them.
- This helps protect our antibiotics so we can rely on them to work when we really need them
- If a antibiotic has been prescribed for a Catheter Associated UTI , your healthcare professional will need to remove your existing urinary catheter and a new catheter replaced after the first dose. You may need to contact your healthcare professional to inform them that you need your catheter changing with the new prescription of antibiotics.
How can I reduce the risk of getting an infection?
- Wash your hands before and after you touch your catheter.
- Do not remove the catheter bag or valves unnecessarily such as when you have a bath or shower
- Avoid the use of talcum powder, perfumed soaps and lotions around the catheter site
- Wash the skin area where the catheter enters the body with mild soap and water at least once a day
Contact information
If you require further information on catheter care during office hours you can contact your health care practitioner or community nurse. If out of office hours please contact NHS 111.
Within the PDF below, there is a section from page 28 onwards for your healthcare professional to fill in for you.