Radiotherapy for Lymphoma (Hodgkin Lymphoma or Non-Hodgkin Lymphoma)
Your oncologist has recommended that you have a course of radiotherapy. This page gives you information about radiotherapy and what will happen during your treatment. Please be aware that our radiotherapy units are training centres for doctors, nurses and radiographers. Students may be present in the department when you have your treatment but they are supervised at all times. If you would prefer not to have students present during your treatment, please let a member of staff know. You may find it useful to write down some questions before you start your treatment.
On this page
-
Radiotherapy for lymphoma
-
What is radiotherapy?
-
How is radiotherapy given?
-
What will happen at my planning scan appointment?
-
What does my treatment involve?
-
Who will I see and when?
-
Side-effects of radiotherapy for lymphoma
-
Self-care during radiotherapy
-
What can I expect after treatment has finished?
-
What support is available?
-
Further information
-
Your data
Radiotherapy for lymphoma
Radiotherapy is a local treatment for lymphoma, this means that it is directed at a specific part of the body.
Radiotherapy may be used when the lymphoma cells are in 1 or 2 areas of lymph nodes in part of the body (stage 1 or 2).
Sometimes radiotherapy is used after chemotherapy, especially if the lymphoma is in just one area of the body, was very large before chemotherapy was given or was in the bone.
For some people with indolent lymphoma in just one area, radiotherapy may be the only treatment. Indolent lymphoma grows and spreads slowly and usually does not have any symptoms.
Radiotherapy can also be helpful in controlling symptoms such as pain, if the lymphoma is more extensive.
What is radiotherapy?
Radiotherapy uses high energy X-rays or other types of radiation to destroy cancer cells. It is also known as radiation therapy or external beam radiotherapy.
The treatment is normally divided into a number of sessions (called fractions), with 1 session given each day for 5 days with a rest at the weekend.
The number of sessions you have depends on several factors including your general health, the type of cancer and the part of your body being treated and whether or not you have received, or you are going to receive surgery or chemotherapy as part of your treatment.
For these reasons, treatment is planned for each patient individually, even those with the same type of cancer may receive different treatments.
Normal cells are also sometimes damaged by the radiotherapy but they can repair themselves more effectively than cancer cells. Side effects occur as a result of damage to normal cells (see pages 11 to 15). Dividing the treatment into fractions helps to make sure that less damage is done to your normal cells than to the cancer cells.
How is radiotherapy given?
Radiotherapy is given using a special type of X-ray machine called a linear accelerator, or ‘linac’. Therapeutic radiographers operate these machines to deliver your treatment.
The radiotherapy is given as a beam focused from outside the body (external radiotherapy). This treatment will not make you radioactive so it is perfectly safe for you to mix with other people, including children or anyone who is pregnant, throughout your treatment.
The machine delivers the treatment by moving around you. It may come close to you but will not touch you. You will not see or feel the treatment but you may hear the sound of the machine moving around you.
What will happen at my planning scan appointment?
Radiotherapy needs to be given in the most effective way, causing the fewest possible side effects. Treatment planning identifies the exact area to be treated. You will normally have a planning scan appointment before your radiotherapy starts. This is so that the team can make a treatment plan for you.
The planning appointment will be done using a CT scan. You will be in the position in which you will have your treatment. This scan is for the sole purpose of planning your radiotherapy and there will not be any results available from it. During the scan, you will need to be in a stable position so that you do not move during your treatment. This will be done using varying pieces of equipment depending on your mobility.
You will be asked to remove any clothing covering the part of the body being treated and lie in your treatment position. You will be in this position for about 20 minutes. During this time, you will need to lie still but you will be able to breathe normally.
The radiographers may draw on your skin with a pen. They may also temporarily stick some markers onto your skin. The radiographers will then need to leave the room to start the CT scan. You will feel the bed move in and out of the scanner. You will pass through the scanner a number of times but will not see or feel anything. The radiographers will then re-enter the room.
Finally, with your permission, the radiographers may make some tiny permanent marks on your skin (referred to as tattoos) using a pinprick of ink. These marks enable the radiographers to accurately position you each day when you have your treatment.
You may not need a CT scan if the area to be treated is in the skin or near the skin’s surface. If this is the case, the doctor may draw marks around an area and photographs may be taken to allow the treatment to be set up in the same position each day.
If you are having treatment to your head or neck, you will need to have a plastic mask made. A mask is required so the radiographers can set you into the same position at each treatment appointment and the position of your head and neck is kept still throughout each treatment.
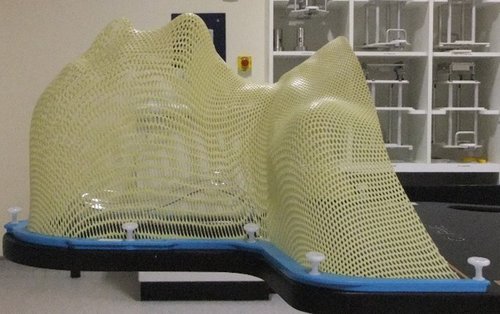
If a mask is needed, you will be given an appointment with the mould room team so that a mask can be made before you have your CT planning scan.
To make the mask a plastic mesh material will be heated up in water until it is flexible. This will be placed over your face and head and gently moulded around you. You will need to lie still for a few minutes until it has set and can be lifted off.
The mask should be quite a tight fit to make sure that you cannot move your head during treatment but it should not be uncomfortable.
What does my treatment involve?
When you attend for treatment, you will be asked to remove any clothing covering the part of the body being treated and then lie on the treatment couch.
The radiographers will position you carefully. This is to make sure you are in the same position as when the treatment was planned. When they have positioned you correctly you will be asked to stay very still but you will be able to breathe normally.
A team of radiographers will work together in the treatment room and you will hear them giving each other instructions and information relating to your treatment. The radiographers will leave the room to switch on the machine. You will only be alone for a few moments at a time. The radiographers will be able to watch you on a closed-circuit TV monitor.
There is also a two-way intercom system enabling the radiographers to talk to you and you can talk to them.
Please remember to stay still at all times so that your treatment is given in the right place. If you need the radiographers, you can move your hand to alert them. They can stop the treatment machine and be with you in seconds.
Treatment only takes a few minutes. The machine may move around you while the radiographers are outside of the room. This is perfectly normal and they will be monitoring you and the machine the whole time.
Who will I see and when?
You may see a Clinical Oncologist (doctor), either a consultant or a specialist registrar. These are doctors who are experts in radiotherapy.
The members of staff you will meet most frequently are therapeutic radiographers. Therapeutic radiographers are specially trained to use the equipment required to plan and deliver the radiotherapy treatment prescribed by your oncologist.
You will see a team of therapeutic radiographers at each treatment session. You may also meet dosimetrists or mould room technicians if you need to have a mask made for treatment.
You may have review appointments during your treatment. The frequency of these will depend on the number of treatments you have. Review appointments provide an opportunity for you to discuss any side effects and your wellbeing during treatment.
You will still have the opportunity every day to discuss any side effects that you have with the radiographers who are treating you, so please do not feel that you have to save up your concerns for the review appointments.
Side-effects of radiotherapy for lymphoma
The majority of side-effects from radiotherapy are predictable, expected and temporary (short term side effects), while other side-effects can be chronic (long term). Everyone’s healing is different so you may find you experience some or all of the following symptoms.
Likewise, you may recover very quickly over a few weeks, or it may take a several months.
Short-term side effects
Radiotherapy has a delayed effect; this means that you usually do not notice any side effects until the end of the second week of treatment. Side effects usually start off mild and will slowly build up during the course of your treatment. They most commonly include:
Tiredness/fatigue
Some patients may find that they feel more tired than usual during treatment (often after 2 to 3 weeks). Travelling to your radiotherapy appointments may also add to this. It is important that you continue with your normal activities and routines as much as possible. Try to find a sensible balance between rest and activity.
Skin reaction
Moisturisers can be used to relieve dry, itchy or red skin caused by treatment. Please ask the radiographers for advice about skin care.
Hair loss
Radiotherapy can cause hair loss in the area being treated. For example, if you have radiotherapy to the lymph nodes in your neck, you may lose the hair on the back of your neck. Radiotherapy to the nodes in the chest may make the hair on your chest fall out. Hair usually grows back after treatment but it can take up to 12 months.
Some side effects from radiotherapy are specific to the part of the body being treated.
Abdomen
Treatment to the tummy area (abdomen) can cause nausea (feeling sick), vomiting (being sick), indigestion, urinary frequency, or diarrhoea.
Head and neck
Treatment to the neck can make your mouth or throat sore and you may develop ulcers inside your mouth. You may also notice that some foods taste different. Your mouth may become very dry during radiotherapy.
Eye
Treatment to the eye can make the eye swollen. The eye may also become very dry or very watery, depending on which part of the eye is treated.
Brain
Radiotherapy to the brain will cause temporary hair loss. You may become very, very tired. At its worst, you may be asleep nearly all the time but this should improve as you recover from treatment. It may cause nausea or vomiting and headaches. There is medication that can help with this, so it is important to mention it to the radiographers delivering your treatment.
Mediastinum (chest)
If you are having treatment to your chest, you may experience a dry, tickly cough. Simple over the counter remedies can help with this, please speak to your local pharmacist. You may also become slightly breathless; if this happens it should improve over a 3 to 4 week period. Sometimes it may be painful to swallow – this can be managed with pain relief such as paracetamol and changes to your normal diet. You should avoid hot spicy food as this can cause irritation. Smoking and alcohol can also cause soreness; it is advisable to avoid both during your treatment.
Loss of appetite
Eating small amounts at regular intervals may help overcome this, try to eat some higher calorie nutritional foods. If you have lost weight or have problems swallowing it may be helpful for you to see a dietician. We may be able to arrange this for you. It is very important to maintain your nutrition during and after treatment to allow the normal tissues damaged by radiotherapy to heal.
Long-term side effects
Late side effects from radiotherapy are again dependent on which part of the body is being treated. They can occur despite our efforts to minimise the radiation dose that they receive. Long-term side effects are less common but can be permanent due to scar tissue forming from the radiotherapy.
Head and neck
After radiotherapy to the mouth, you might develop dental problems or a long-term dry mouth. Radiotherapy to the neck can slightly increase your risk of strokes some years after radiotherapy. It can also make your thyroid gland underactive some years after radiotherapy.
Eye
When the lens of your eye becomes misty or fogged, making it difficult to see clearly, this is called a cataract. Your specialist will shield your lens from the radiation beam if possible. A cataract after radiation exposure takes a while to develop – sometimes years. If you do get a cataract, you can have an operation to remove it and put in a new lens. You may also develop a dry eye after radiotherapy. Drops can be used to moisten the eye if this becomes a problem, these can be discussed with you if necessary and are available from pharmacies.
Groin or armpit
If the lymph nodes in the armpit or groin become damaged by radiotherapy, fluid can build up in your arm or leg. This is called lymphoedema and is rare. Your consultant or GP can give you advice about how to manage lymphoedema.
Brain
Radiotherapy to the brain can cause difficulties with concentration and memory some years after radiotherapy.
Mediastinum
Depending on where the cancer was in the chest, radiotherapy may cause a slightly increased risk of angina and heart attacks in the long term. The risk is very small and every effort will be made to reduce this as much as possible with the radiotherapy planning.
Radiotherapy can sometimes cause scarring of the lungs (fibrosis). This is not usually a problem if the rest of your lungs are healthy, but it may be seen on CT scans.
Heart
Radiotherapy may cause a slightly increased risk of angina and heart attacks in the long term. The risk is small. Every effort will be made to reduce the risk as much as possible with the radiotherapy planning.
As the treatment involves using radiation, there is a very rare risk that it may cause another cancer in the future, within the area treated.
Self-care during radiotherapy
Try to allow time for rest. Everyone reacts differently, and as treatment progresses you will get an idea of the effect it is having on you.
Skin care in the treatment area
- Moisturise frequently. Use a moisturiser you prefer and like. If you do not currently use a moisturiser, please speak with your radiographers as they will be able to suggest some options.
- If a moisturiser is causing irritation, stop using it and discuss it with your radiographers.
- Avoid sun exposure to the treatment area – wear a brimmed hat and/or cover up with clothing. You should continue to protect your skin from direct sunlight after your treatment has finished by covering the treated skin and using a high SPF sunscreen or sunblock. The treated skin will remain more sensitive to the effects of sun exposure.
- Wash your skin gently with soap and water and gently pat dry with a soft towel. You may shower or bath as normal. Your skin may be more sensitive than usual, so do not have the water too hot.
- If your head or neck is being treated, we advise you to wash your hair gently with your usual shampoo. If you use a hairdryer, it should only be on a cold setting.
- Swim if you wish, as long as the skin is not sore or broken but shower and dry the area carefully afterwards.
- Try to avoid exposing the treated area to extremes of temperature, such as heat pads, hot water bottles, saunas and ice packs during radiotherapy and in the following few months.
Please avoid rubbing the area, using sticky tape, wet shaving, wearing make-up and using wax, hair removal cream or lasers.
Health and wellbeing
- Keep well hydrated – aim to drink 2 litres (4 pints) of water a day.
- Avoid drinking alcohol.
- Eat a nutritionally well-balanced diet.
- Keep active if you can – activity helps to improve outcomes and help you cope better with any side-effects.
What can I expect after treatment has finished?
Radiotherapy has a delayed effect in which the side-effects will continue even after your treatment has finished. Side effects tend to reach their peak around 7 to 14 days after your last radiotherapy session, so do not be alarmed if they worsen.
Recovery times vary from person to person, but side effects should gradually improve over the following 6 to 12 weeks.
You will be given regular appointments with your oncologist or haematologist over the next few years. If at any time between appointments you are concerned about something, please contact your GP or the hospital via your Clinical Nurse Specialist (CNS) team so that an earlier appointment can be made if necessary.
It is not unusual for people to be anxious about the possibility of the cancer recurring, and it might be better for you to seek advice rather than worry.
Remember that everyone is different and may react differently to treatment. You will have met many other people having radiotherapy during your visits to the department but their treatment may have been very different from yours, so their experience should not be compared.
What support is available?
Many people, quite naturally, feel emotionally upset and frightened following the diagnosis of cancer. It may be difficult to adjust to what is happening. Finding out as much as you can about your treatment may help to calm your fears and allow you to cope better.
The therapeutic radiographers and other healthcare professionals you may meet will be willing to listen to your worries and support you in any way they can. They may be able to refer you to support services offered in your hospital.
Further information
Further information is readily available online, we would recommend beginning with:
Macmillan Cancer Support
Tel: 0808 808 0000
Website: www.macmillan.org.uk
Cancer Research UK
Website: www.cancerresearchuk.org
Lymphoma Action
Helpline: 0808 808 5555
Website: https://lymphoma-action.org.uk/
Further support will be available locally, please speak to your oncology team who can advise what local charities are there to help you and which support groups are available near you.
The links will direct you to further resources relating to your radiotherapy treatment. You can type in the web address into your internet browser:
The Society and College of Radiographers: Radiotherapy Skin Reactions
Website: Website: www.sor.org/getmedia/e091da21-6dc8-47fb-9e08-094a0cb3135e/5056_-_sor_design_doc_a_patient_infosheet_-_skin_care_a5_leaflet_llv2-1_2.pdf
Macmillan: Understanding Radiotherapy
Your data
All personal images and photographs taken during your radiotherapy will be used in accordance with the local Trust policy on the protection and use of patient information.
To read more about the Privacy Policy for Gloucestershire Hospitals NHS Foundation Trust, please visit: