Total Laparoscopic Hysterectomy (TLH)
This page gives you information about having a Total Laparoscopic Hysterectomy (TLH). It also answers some of the commonly asked questions.
On this page
-
What is a TLH?
-
Why am I having a TLH?
-
Before the surgery
-
Pre-operative assessment
-
Will I have to sign a consent form?
-
When should I stop eating and drinking?
-
Day of the surgery
-
During the surgery
-
After the surgery
-
Risks
-
Benefits of the surgery
-
Will I need a catheter?
-
When can I resume my normal diet?
-
How long will I be in hospital?
-
Follow up
-
Going home
-
Returning to normal
-
When can I go back to work?
-
What about my sex life?
-
When can I drive?
-
Will I need hormone replacement therapy (HRT)?
-
Contact information
What is a TLH?
TLH is a major surgical procedure which involves removing the uterus and cervix using keyhole (laparoscopic) surgery. Ovaries and fallopian tubes may or may not be removed depending on the reason for surgery. If the ovaries are removed, depending on your age, you will start the menopause (change of life).
This surgery may be combined with other procedures, such as repair of a prolapse or removal of pelvic lymph nodes, if it is being performed to treat a cancer.
Hysterectomy can be carried out vaginally, abdominally, laparoscopically or in a combination of these. TLH may reduce your recovery period (including hospital stay), reduce the pain and discomfort you experience after the surgery but can have a higher risk of complications, particularly urinary tract injury.
Why am I having a TLH?
Common reasons for TLH surgery include painful or heavy periods, pelvic pain, fibroids, prolapse, endometrial or early-stage cervical cancer. Your doctor will explain why you are having this surgery.
Before the surgery
You should carry on taking your usual medications, unless told otherwise.
We strongly advise that you stop smoking before your surgery. If you develop an illness before your surgery or have any questions, please contact your consultant’s secretary.
Pre-operative assessment
You will be invited to the hospital any time up to 2 weeks before your surgery for a pre-operative assessment.
During this assessment we will check your fitness for a general anaesthetic and the surgery. This will include recording a full medical history, your current medication and arranging any investigations required.
Please tell the nurse practitioner or doctor if you have had problems with any previous surgery, anaesthetic or if you have any allergies – this is very important.
At this visit you will have the opportunity to discuss what to expect before, during and after the surgery. We will also tell you what you will be able to do during your recovery time.
Your admission details will be confirmed with you during this visit.
Will I have to sign a consent form?
You will be asked to sign a form giving your consent to the surgery. The consent form gives your gynaecologist the right to do only what is written on this form.
The only exception to this is if during the surgery there is an unforeseen problem, you have then consented to have this corrected. Please feel free to ask any questions about the surgery that you do not understand before signing the consent form.
The medical terms commonly used on the consent form are:
- Total Laparoscopic Hysterectomy (TLH) - removal of the womb which includes the cervix (neck of the womb).
- Oophorectomy - removal of one ovary.
- Bilateral oophorectomy - removal of both ovaries.
- Salpingectomy - removal of one fallopian tube.
- Bilateral salpingectomy - removal of both fallopian tubes.
- Salpingo-oophorectomy - removal of one ovary and fallopian tube.
- Bilateral salpingo-oophorectomy - removal of both ovaries and fallopian tubes.
When should I stop eating and drinking?
Detailed instructions will be included in your admission letter about when to stop eating and drinking. It is very important that you follow the instructions otherwise your surgery may need to be put off until a later date. This will be discussed at your preoperative assessment appointment.
Day of the surgery
An anaesthetist and your surgeon (or a senior member of the team) will explain to you what will happen during your operation.
We want you to fully understand why you are having the surgery and what the possible risks are. You will be asked to sign a consent form, if you have not already done so. You will also have the opportunity to ask any questions that you may have.
During the surgery
TLH is normally carried out under a general anaesthetic (while you are asleep). A narrow plastic tube called a cannula will be inserted into a vein in your arm or hand using a needle; this is used to give you fluids and medications.
After you have been given a general anaesthetic and you are asleep, a catheter (a tube for urine drainage) will be inserted into your bladder.
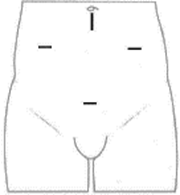
A small cut (about 2 cm) will then be made under your navel (belly button). The abdomen will be filled with gas and an optical instrument, called a laparoscope, will be inserted to allow the internal organs to be viewed before 3 further small cuts, about 1 cm each, are made on your abdomen. These cuts are for other instruments to be inserted.
Your ovaries and fallopian tubes may or may not be removed depending on the reason for your surgery. In most cases the uterus and cervix are removed through the vagina. If the uterus is too large to remove vaginally, or the vagina is too narrow, a slightly larger cut will be made on the abdomen and it will be taken out that way.
The wounds will be closed with dissolvable stitches.
The procedure takes about 1 to 2 hours, but you can expect to be in theatre and recovery for 3 to 4 hours.
After the surgery
You will normally wake up in the operating theatres recovery area, but you may not remember much until you are back on the ward. You will be given medication during the surgery to relieve the pain when you wake up. You may have some discomfort following the surgery but we will try to control this in the best way possible using a variety of pain relief.
Risks
Minor risks
- Inflammation, infections and bruising to any wound on the abdomen or in the vagina.
- Haematoma (blood collecting in the wound).
- Chest infection.
- Urinary tract infections such as cystitis may happen in about 1 in every 6 women.
- Hernia.
- Adhesion (tissue sticking together).
More serious risks
- Injuries to the bladder, ureters (narrow tubes between the bladder and the kidneys), bowel or blood vessels, requiring further surgery, a blood transfusion or a longer admission.
- Blood loss can sometimes be heavy during the surgery and this may mean that you will need a blood transfusion.
- Anaesthetics carry a small risk and you will be asked by your doctors about any medical problems that might increase those risks.
- Thromboses (blood clots in the leg or chest) are uncommon after this surgery. Preventative treatment will be discussed.
Benefits of the surgery
- Less pain after the surgery than having ‘open’ (traditional) surgery.
- Fewer wound complications.
- Less disruption to bowel and bladder function.
- Lower risk of Deep Vein Thrombosis (DVT).
- Shorter recovery period compared to other forms of hysterectomy surgery.
Will I need a catheter?
Immediately after a hysterectomy some women find it difficult to pass urine. The catheter mentioned earlier on this page, allows the bladder to stay empty until you are completely awake from the anaesthetic and more mobile.
The catheter is usually removed the day after surgery.
When can I resume my normal diet?
You may be able to have a drink a few hours after your surgery, until then you will be given fluids via the cannula in your arm. You will usually be eating and drinking normally within a day of the surgery.
How long will I be in hospital?
You will be discharged 1 or 2 days after the surgery. If you have had additional surgery, you may be in hospital for a longer period.
If you have any concerns about going home after the surgery, please discuss these with the staff at the Pre-operative Assessment Clinic.
Follow up
You may be given a follow-up appointment at the hospital or you will be asked to make an appointment to see your GP.
Going home
You may still have some discomfort when you leave the hospital but you will be given a supply of pain relief medication. This should be taken regularly for the best effect. You may also be given laxatives to take home, as minor bowel problems are common after hysterectomy.
After the surgery you may experience ‘wind pains’, this is due to having medical air inside your abdomen during the operation. These pains should stop within a few days. Drinking a small amount of peppermint oil in warm water can help. Peppermint oil can be bought in supermarkets and health food shops.
You may notice some weight gain during the first few weeks following surgery this is because you are less active. Hysterectomy itself does not cause weight gain.
You may have some light vaginal bleeding (spotting) for up to 6 weeks after the surgery, this is normal.
If the bleeding becomes heavy, has a bad smell or if you are concerned, please contact your GP.
Returning to normal
You may feel more tired in the weeks following your surgery if you do too much.
You may also experience a slight aching discomfort at the wound sites. In some cases, this can carry on for some months after the surgery. Most women are able to resume normal activity in terms of exercise and daily tasks within 4 to 8 weeks.
It is advisable not to swim until all the wounds have healed and any vaginal discharge has cleared up.
When can I go back to work?
We suggest that you stay off work for 4 to 8 weeks; this will depend on the nature of your job. Please discuss this with your consultant or GP.
What about my sex life?
The area at the top of the vagina where the cervix was will have stitches which will need about 6 weeks to heal before intercourse is resumed. You will tend to know when you feel ready to resume intercourse. You should find that there is no alteration in the sensation but there may initially be slight discomfort if you are over enthusiastic. If you experience any pain, please seek advice from your GP.
When can I drive?
You should not drive until you feel able to perform an emergency stop comfortably and are not taking regular pain medication. This usually means about 6 weeks without driving. We recommend that you discuss this with your insurance company.
Will I need hormone replacement therapy (HRT)?
HRT will have been discussed with you in the Out-patient Clinic before the surgery. Whether HRT is offered to you will depend on whether your ovaries are removed during the surgery and your age.
- If you have not yet reached the menopause and your ovaries are left in place, there is a possibility that they may stop working at an earlier age than normal. If you do develop hot flushes or other menopausal symptoms before the age of 45 you should seek advice from your GP about the possible need for HRT to prevent osteoporosis (premature thinning of the bones).
- If your ovaries are removed at the time of the hysterectomy, before you reach the menopause, you will be offered oestrogen replacement therapy until the age of 50. This will depend on your diagnosis.
- If you have already reached the menopause before the surgery, your need for HRT will not change. If you were not taking it before the surgery, you should not need it afterwards.
- You may wish to discuss the advantages and possible disadvantages of HRT with the gynaecology team or your GP before or shortly after your surgery.
If it has been decided that you will need HRT you will be given a month’s supply to take home, after that further supplies can be obtained from your GP.
Contact information
If you have any problems or concerns after going home, please contact your GP for advice.