Tracheostomy
The doctors looking after you/your family member are considering performing a tracheostomy. This is to help with your overall treatment while you are a patient in the Department of Critical Care (DCC). We have written this page to give you information about having a tracheostomy. It explains what a tracheostomy is, what the procedure involves and the possible risks. We hope that it will help to answer some of the questions you may have. If you have any further questions or concerns, please speak to a member of the Critical Care team.
What is a tracheostomy?
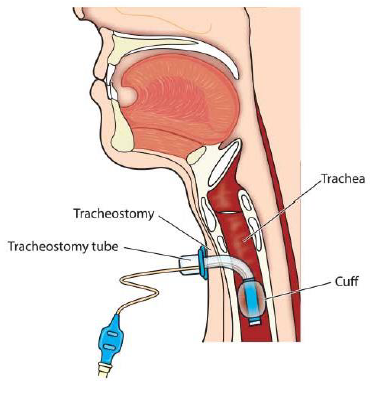
A tracheostomy is an opening (stoma) created at the front of the neck to allow a tube (called a tracheostomy tube) to be inserted into the windpipe (trachea) to help with breathing. This tube creates an artificial airway which allows you to breathe through the tube (rather than through your nose or mouth). If necessary, the tube can be connected to an oxygen supply and a breathing machine called a ventilator.
A tracheostomy is a small operation and is usually performed in the DCC by one of the senior intensive care doctors. You will be given a general anaesthetic so that you are asleep and unaware of the procedure. In some cases, this procedure is performed in theatre.
Benefits of having a tracheostomy
- A tracheostomy can be a lot more comfortable than a tube in the mouth and makes it easier to breath while on the ventilator.
- The tracheostomy will allow sedation to be reduced. This means you/ your family member are more likely to be aware and therefore reduces the risk of the complications such as delirium (an acute onset of confusion) associated with the sedative medications given.
- A tracheostomy allows easier removal of chest secretions while you are ill and helps with the recovery of your lungs.
- A tracheostomy can help with communication as you are often awake.
Risks of having a tracheostomy
- Bleeding either at the site of the tracheostomy or into the windpipe.
- Infection.
- Blockage of the tube. We minimise this risk by having an inner tube which is removed and cleaned regularly.
- Displacement of the tracheostomy tube, the highest risk is during the first 48 hours. This has to be balanced against the accidental displacement of the oral tube already assisting with the breathing.
- There may be some narrowing of the trachea. In extreme cases this could cause long term problems with the breathing and make it hard to breath without a tracheostomy. Surgery may be needed to widen the airways which may involve inserting a small tube called a stent to keep the airways open.
Rarely, the complications listed above may be very serious and even result in death. The consultants looking after you believe this risk is small in comparison to the benefits you will receive.
Care of a patient with a tracheostomy
Oxygen and humidification
Oxygen or support with the breathing via a ventilator (breathing machine) will be given via the tracheostomy tube rather than via a face mask.
The flow of oxygen can be quite drying to the lungs and airways so the oxygen will be humidified (water vapour) and warmed via our equipment. This will improve the comfort and loosen any phlegm making it easier to cough or suction off. You may also have regular nebulisers to help with this.
Coughing and suctioning
You/your family member will be encouraged to breathe deeply and cough regularly. You should also perform the breathing exercises you have been shown by the physiotherapist. This will help to prevent further chest complications and work towards the removal of the tracheostomy. The physiotherapist will continue to see you while you have the tracheostomy in place to help in gradually increasing the amount of time off the ventilator until you are able to manage without the ventilator.
Communication and speaking
Most tracheostomy tubes have an air filled cuff around the tube. When the cuff is inflated, you/your family member will not be able to speak. This is because the air cannot pass through your vocal cords.
We are aware that being unable to speak can be frightening and frustrating. To help with this, we may ask you/your family member to try and write things down or use gestures to let us know what you want.
As your condition improves, we will gradually remove the air from the cuff. This will allow air to pass through the vocal cords so you can begin to speak. We may also try a ‘speaking valve’ (device used to help more air pass through your voice box to make your voice louder). Patient Information
Eating and drinking
While the tracheostomy tube is in place it may affect your ability to swallow. Therefore, initial attempts at drinking will be supervised by nursing or physiotherapy staff. If there are problems with your swallowing, then you will be referred for a swallowing assessment. If your swallow has been affected, you may be asked to wet your mouth with water rather than drinking.
If you/your family member find it difficult to eat and drink enough, a small feeding tube will be passed through your nose and into your stomach. This is normally a short-term measure and will not cause any long-term complications. The tube can be used to give fluids, medications and liquid food with added nutrients directly into your stomach.
While the tracheostomy tube is in place, your sense of taste and smell may be altered. This usually returns to normal once the tracheostomy tube is removed.
Removing the tracheostomy tube
Most tracheostomies are temporary. Usually, the tube is removed when the reason for its insertion has resolved, and you/your family member have regained sufficient strength to be able to breathe deeply and to cough effectively. The decision of when to remove the tube will be made by the Intensive Care Team/Outreach Team and the physiotherapist.
Removal of the tracheostomy tube can be done on the ward, sedation or anaesthetic will not be needed. Removing the tube takes less than 5 seconds but will leave a small hole in your neck. A dressing will be placed over this hole until it has healed.
After the tracheostomy has been removed you will find that air and phlegm continue to come out through the hole. This is completely normal and not a sign that something has gone wrong. Within a few days the hole will start to heal over, and any phlegm should stop leaking.
In the meantime, when coughing or talking, try to support the dressing by covering the hole with your fingers to prevent air leakage. The wound (hole) will be re-dressed as necessary.
You may still need oxygen and physiotherapy after the tracheostomy tube has been removed. Patient
Frequently asked questions
What if the patient is unable to give consent?
If your family member is sedated or too unwell to agree to the tracheostomy, we will discuss the procedure with the family. We can also make decisions about the care when we feel it is in the patient’s best interest. If this is the case, we will speak with the next of kin before making a final decision.
Who will care for me/my family member?
You will be cared for by multiple teams, including doctors, nurses, physiotherapists, speech and language therapists, dietitians, critical care nurses and anaesthetists.
How long will I need to have the tracheostomy tube in place?
This will depend on the reason for having a tracheostomy tube put in. Some people may only need the tube for a few days, whereas other people may need the tube for much longer. We will discuss this with you.
If the tracheostomy tube is permanent, we will show you and your family or carers how to look after the tube. Before you leave hospital, we will also show you what to do if the tube moves or becomes blocked.
You will be given an appointment date to have the tube changed. This will be as an outpatient.
What if there is a need to have the tracheostomy tube changed?
We may need to change your tracheostomy tube if has been in place for 28 days or a different tube is needed to help with breathing and talking as you/your family member get stronger.
There is no need for sedation to have the tube changed. It is a quick procedure and will usually be performed by a doctor on the DCC unit.
If you have any further questions, please do not hesitate to ask.
Acknowledgment
With grateful thanks to:
- Dr Sahil Gupta, Clinical Fellow, Anaesthesia and Critical Care, Gloucestershire Hospitals NHS Foundation Trust.
- Dr Simon Webster, Clinical Lead for Critical Care, Consultant in Anaesthesia and Critical Care, Gloucestershire NHSFT.