Trans Urethral Resection of the Prostate (TURP)
This page is for patients about to have a Trans Urethral Resection of the Prostate (TURP). Over 45,000 TURP operations are carried out each year in the United Kingdom, 350 of these are performed at Gloucestershire Hospitals NHS Foundation Trust. This surgery is carried out at Cheltenham General Hospital. Other operations for enlargement of the prostate are available.
Definition
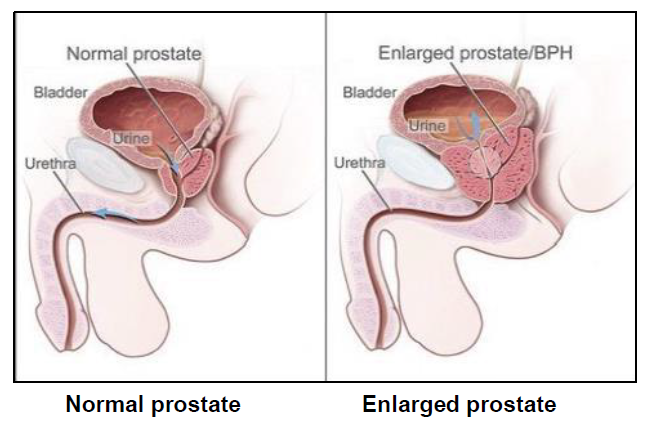
The prostate is a gland that only men have, which sits around the urethra (water pipe) just beneath the bladder. It produces the fluid part of a man’s semen (also known as ‘the ejaculate’). TURP is an operation carried out on patients who have developed an enlarged prostate.
As the prostate enlarges, it squashes the urethra (a bit like putting your foot on a hosepipe) and this stops the bladder from emptying properly. If this is left untreated the bladder may continue to fill with urine, which could lead to a build-up of pressure which can cause damage to the kidneys.
This problem can occur in men aged below 60 years, but it becomes more common in men aged over 60.
About half of men aged around 60 will have an enlargement of the prostate. This number rises to around 5 out of every 6 men aged 80 and over.
Enlargement of the prostate is not cancerous (known as benign) in around 85 out of every 100 cases. Any prostate tissue taken away during surgery will be analysed to rule out cancer.
TURP is the removal of the central part of the prostate gland using heat diathermy through a narrow telescope put into the urethra. The tissue is cut using an electrical current that heats a wire at the end of the telescope to cut the prostate tissue and reduce bleeding. State of the art bipolar energy is now used routinely for this surgery in Gloucestershire.
This operation will be done under spinal or general anaesthetic and usually takes 30 to 60 minutes, depending on the size of the prostate.
A catheter will be placed into the bladder following surgery.
TURP is most commonly done as a day case operation. You should bring an overnight bag as some patients do need to stay in hospital following surgery. However, you should plan to have a responsible adult available to take you home and stay with you over night.
There are no cuts (also known as incisions) made in your abdomen during the operation, so you will not have any scars that show.
The prostate can re-grow and it is important to note that if this happens, you may need to have the operation again. Around 10 in every 100 patients need to have the surgery again, usually about 8 to 12 years after the first operation.
Benefits
The benefits we usually expect from this operation are:
- An improvement in the flow of urine.
- Less frequent and less urgent passing of urine.
- Fewer visits to the toilet at night time to pass urine.
- If you have a permanent urethral catheter, it will be taken out.
It is important to note that your symptoms may have taken years to develop and may take several months to settle down completely after the operation.
Risks
Incontinence (leaking urine)
Less than 1 in every 100 men having TURP have problems with incontinence after the operation. Some men find they need to empty their bladder more often, with urgency and ‘urge leakage’ following the surgery. This is due to the bladder becoming irritable as a result of the blockage at the prostate.
Most patients with an irritable bladder will find that their symptoms improve over the first 3 months after the operation. Bladder re-training can be useful and in some cases medication may also help.
Impotence (inability to have an erection)
As few as 14 in every 100 men having TURP experience new problems getting an erection (impotence) after the operation. If you decide to have this operation and impotence becomes a problem afterwards, please see your GP or discuss this at your follow-up telephone or clinic appointment. We have experienced practitioners who deal with this problem and can offer advice and treatment where needed.
Retrograde ejaculation (the ejaculate goes backwards into the bladder)
During the operation, the valve (sphincter) that stops the ejaculate going backwards into the bladder may be affected. This happens in 70 out of every 100 men who have had TURP; this is a permanent condition.
During intercourse and climax, the majority of the ejaculate (semen) goes backwards into the bladder.
It will remain in your bladder until you next pass urine. This will not harm you, but it can affect your enjoyment of sex and can feel rather odd. It can also affect your ability to father children, but it should not be used as a form of contraception, as there is always a risk of some of the ejaculate coming out in the usual way.
A retrograde ejaculation sparing technique is possible in some patients and we plan to offer this soon at our hospitals.
If this concerns you an alternative procedure may be available.
Bleeding
Most surgical operations carry a risk of bleeding. We will take a sample of your blood and save the specimen in order to be able to give you a blood transfusion if needed, although the risk of this is low.
1 in every 100 patients need to go back to theatre due to bleeding.
It is normal to see some blood in the urine for the first
1 to 2 days. Constipation can increase the risk of bleeding after TURP, as straining or passing a hard stool can cause pressure on your prostate. We advise that you try to eat a high-fibre diet with plenty of fruit and vegetables before and after the operation.
You will also need to drink about 2 litres of fluid (10 cups per day) after the operation, while you are in hospital and for about 3 to 4 weeks after you go home. This will make sure that any debris in your bladder is washed out and it will help you to pass good amounts of urine.
Perforation
In rare cases, a hole may be made through the prostate. If this happens, urine could leak into the pelvis, so a catheter is left in place until the hole has had time to heal.
Infection
Putting anything into the bladder carries the risk of infection, no matter how sterile the procedure. Signs of infection are frequency, urgency and having severe burning when passing urine, you may also have a raised temperature. You may feel the need to pass urine, even when there is no urine in your bladder.
If you have an infection during your stay in hospital, you will be given antibiotics. If you continue to have all or some of these symptoms after discharge, please see your GP urgently.
Please note that the first few times that you pass urine after the operation, you may find it quite sore and/or painful. At first you will probably notice some frequency and urgency of passing urine. This may take several months to settle down completely.
Before the operation
In the pre-admission clinic, we will check that you are fit and well enough to have the operation.
You will be given instructions about diet; you will also be advised on what items to bring in to hospital.
You should also arrange for an adult to be with you for the
24 hours following your discharge. If this is not possible, please make sure that the nursing staff are aware before the operation so they can begin making any additional arrangements needed for your discharge.
On the day of your operation
You will not be able to eat or drink for 6 hours before your operation (this includes chewing gum). This is to make sure that we can safely give you an anaesthetic.
An anaesthetist will see you before your operation and check to see if you are well enough to have an anaesthetic. There are generally 2 types of anaesthetic that are used for this operation, general anaesthetic (while you are asleep) and spinal anaesthetic. These will be discussed with you, and the anaesthetist will decide which one is safest for you, taking your medical history into consideration.
After the operation
During the operation, a drip will have been inserted into a vein in your arm to give you fluids. You will also have a catheter in your urethra; this is a tube to drain urine from your bladder. The catheter is held in place by an internal balloon which will stop it from falling out.
Your urine may be quite bloody after the operation. This is normal. The prostate has thousands of tiny blood vessels supplying it. In order to stop the bleeding, the blood vessels are sealed (cauterised) as the prostate is cut away, but it is difficult to seal all of these.
Day case
At the end of the procedure the surgeon will decide if same day discharge is possible. A catheter will be placed and often the urine is only lightly stained with blood. Irrigation fluid is usually not required. You will be discharged following a period of observation. Normally you will be given an appointment for the removal of the catheter before leaving the hospital.
Inpatient
Some patients need to stay in hospital for bladder irrigation, typically this is for 12 to 18 hours after the operation. The catheter will have irrigation fluid going into it in order to wash the bladder out and prevent blood clots blocking the exit of the bladder. When the urine starts to clear, the irrigation will be stopped and the catheter is usually taken out 18 to 24 hours later. You will then stay in hospital until we are sure that you are passing urine with a reasonably good flow. Nursing staff on the ward will scan your bladder with an ultrasonic scanner (this is painless), in order to make sure that you are emptying it properly.
Up to 18 out of every 100 patients will find that their first trial without a catheter is not a success. If this happens, we will send you home with a catheter. You will be shown how to look after the catheter.
Arrangements for the catheter to be taken out will be made for about 2 weeks after discharge.
At home
On discharge from the hospital, you should have an adult with you for the first 24 hours in case you have any difficulties passing water or with bleeding. If this is not possible, please make sure that the nursing staff are aware of this.
Bleeding
Following discharge from hospital it is normal to have some blood in the urine. About 2 weeks after the operation, the scabs on the prostate will come away and you may have some bleeding. This may happen on and off for up to 3 months after the operation. Please note that if the bleeding becomes heavy and clotted, there may be a risk that a blood clot will block the exit of the bladder and you would not be able to pass urine. Please contact your GP if you are concerned.
Driving
Do not drive or do any heavy lifting for 2 weeks. If you do drive and have to brake suddenly or if you lift a heavy object, you may cause bleeding from the prostate. This may result in you being admitted to hospital.
Sex
It is safe to have sex 4 weeks after your operation, although climax may feel different due to the retrograde ejaculation mentioned earlier. Some men experience pain or discomfort for the first few times.
Time off work
We suggest that you are off work for 2 weeks. We will give you a fitness to work certificate when needed.
Alternatives to TURP:
Medication
- Alpha blockers, for example tamsulosin, help to relax the bladder neck muscle to improve flow. Side effects include retrograde ejaculation in 7 out of 100 patients, low blood pressure and difficulty getting an erection.
- 5-alpha reductase inhibitors, for example finasteride, which reduce the size of the prostate gland by 20 to 30%. Side effects include difficulty with erections.
Surgery
Aquablation - The procedure involves an ultrasound in the rectum and treatment with a water jet via a telescope in the urethra. This procedure is good for patients with medium to large prostates and those with particular concerns with regard to continence and post operative sexual function. Patients will require a general anesthetic and most go home the same day. A catheter is left in place at the end of the procedure. The procedure takes 45 to 60 minutes. We have a surgeon who performs this procedure at Cheltenham General Hospital.
Urolift® - This procedure involves passing implants into your prostate, via your bladder, using a telescope. The implants are placed between the inner and outer surfaces of the prostate so that they pull the obstructing prostate lobes away from your urethra. The procedure usually takes 30 minutes and patients go home the same day. We have a surgeon who performs this procedure at Cheltenham General Hospital.
Laser surgery
This is a procedure to remove parts of the prostate via a telescope in the urethra and is done under general or spinal anaesthetic in a similar way to TURP. A laser is used to cut the enlarged prostate away. A catheter is left in place at the end of the procedure. The procedure usually takes 45 to 90 minutes. The catheter is removed the following morning. We have a surgeon who performs this procedure at Cheltenham General Hospital.
Robotic Prostatectomy for non-cancer
This procedure involves a robot assisted approach via key hole incisions in the abdomen. This procedure is used for patients with very large prostates, where a TURP or other surgery is unlikely to be successful. We have a surgeon who performs this surgery.
Other options may be available and these can be discussed with your surgeon during an outpatient appointment.
Further sources of information
The British Association of Urological Surgeons (BAUS) - patient leaflet
Website:
www.baus.org.uk/patients/information_leaflets/category/8/prostate_procedures
Decision support tool: making a decision about enlarged prostate (BPE)
NHS Choices’ TURP information page and video:
Website: www.nhs.uk/Conditions/resectionoftheprostate/Pages/Introduction.aspx
Contact information
If you have any further questions or problems following your operation, please contact your GP or the:
Advanced Nurse Practitioners for Urology
Cheltenham General Hospital
Tel: 0300 422 5193
Monday to Friday, 8:00am to 5:00pm