Treating your leg ulcer
The information on this page answers many of the commonly asked questions about leg ulcers. If you have any further questions about your condition or treatment, please feel free to ask at your next clinic appointment or the next time you see your primary care nurse.
About leg ulcers
Leg ulceration is a common problem affecting about 1 to 2 people in every 100 in the United Kingdom.
Leg ulcers can appear suddenly or as a result of an injury to the leg. They are defined as leg ulcers if they do not heal within 2 to 4 weeks.
Most leg ulcers are venous in origin. This means that they are caused when there is a problem with some of the veins or muscles in the leg returning blood to the heart. Every time your leg muscles move, they help pump the blood back towards the heart while a series of valves in your veins stop the blood from flowing backwards.
Problems begin when the valves or muscles become damaged or weakened and are unable to stop the backflow of blood. Due to gravity, this causes an increase in pressure in the veins of the lower leg as the blood struggles to return back to the heart. Eventually, fluid and blood cells are forced out into the surrounding tissue. This leakage is toxic to the skin and can cause it to break down or can delay wound healing.
Treatment
In recent years, research into the treatment of leg ulcers has resulted in more ulcers healing and remaining healed than in the past. The main reason for this success is the development of new techniques in assessment.
An assessment of the circulation in your leg will give us the information to start the appropriate treatment. Treatment will be aimed at treating the cause of the ulcer rather than just the wound itself. Appropriate treatment for leg ulcers caused by poor circulation in the veins is aimed specifically at helping those veins to pump blood back up the leg more effectively.
If you are referred to the Gloucestershire Leg Ulcer Service you will attend one of the Vascular Laboratories in order to have a full assessment of your circulation. During your assessment you will have an ultrasound scan on your veins. This is called a Duplex. You will also have a test to check the condition of your arteries called a Doppler.
Your treatment will be continued by your community nurse or the nurse at your GP’s surgery. You will also be monitored closely at the Leg Ulcer Clinic in a hospital near to your home.
As well as the treatment, there are many steps you can make to help your ulcer heal and stay healed.
Elevation
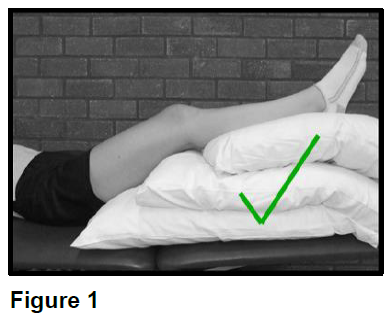
Elevation is one of the most important aspects of the treatment of your leg ulcer. Elevating (raising) your legs to above the level of your heart encourages the blood to return to the heart and reduces backflow in the veins. This will help the healing process.
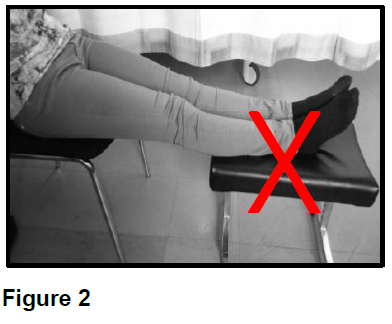
Elevating your legs on a stool while sitting in a chair, or in a recliner chair where your legs are out straight will not help the blood to return to your heart. The most effective way to help the blood return to your heart is to lie down with your feet above the level of your heart. Please see Figure 1 and Figure 2 on the next page.
We would advise you to elevate your legs in this position for at least 2 hours in the morning, afternoon and evening - a total of 6 hours a day. This will often require you to change your normal daily routine.
Exercise
Keeping active is another important function to healing your ulcer. The action of walking causes the calf muscle to squeeze the veins and pump the blood back towards the heart. Without this pumping action, all the blood will continue to collect in your legs due to gravity.
Try to avoid standing for long periods of time, for example when ironing, cooking and washing-up.
If you do find yourself in a situation where you need to stand, try walking briskly on the spot or lifting your heels. This will help to keep your blood circulating.
Compression bandages
After your assessment at the Leg Ulcer Clinic, your treatment will be explained to you. This treatment may involve wearing a compression system. This is usually done with the use of specialised bandages. These bandages will help the healing by gently squeezing the blood up the veins in your leg. This will prevent backflow and swelling.
Multi-layer compression bandages
The multi-layer system is the ‘gold standard’ treatment for venous leg ulcers and has been designed for comfort and healing. Here are some of the benefits for using the multi-layer bandage system:
- The system allows the compression to be gradually increased to reach the correct compression levels.
- The dressing will only need to be changed once a week in most cases. If your ulcer is very wet this may need to be more often.
- The bandages are comfortable even on the most difficult shaped limb. They are flexible and should not provide problems when walking.
- The layer of the bandage that comes into contact with the skin is made from natural fibres. This reduces the risk of an allergic reaction.
Short stretch compression bandages
The short stretch bandage system is a 2 layer bandage method; a padding/reshaping layer and a high compression layer.
Adjustable compression device/compression wraps
These are compression garments which can be applied and adjusted by the patient. They usually consist of Velcro® straps that wrap around the leg to provide compression. These garments will need a separate dressing to be applied to the ulcer underneath. The appropriate dressing will normally be prescribed by your nurse who will advise you on the frequency of dressing changes.
Compression hosiery kits
These kits consist of 2 stockings. The first one is a liner which gives very light support. The outer stocking is applied over the top of the liner. This second stocking is a firmer support and the two together should give an equivalent level of compression to the bandages and wraps.
What to do after your assessment
After your assessment, any treatment planned will be discussed with you. Compression bandages are usually changed by your community nurse or your GP’s practice nurse once a week.
If you experience any of the symptoms listed below you should remove the bandage and seek advice from your nurse, GP or one of the specialist nurses at the Leg Ulcer Clinic. Out of normal surgery hours you should contact your on-call district nurse or NHS 111.
- Pins and needles in your feet or toes
- Blue or white coloured skin on your toes
- Swelling in your toes
- Unusual pain in your leg, foot or toes
- Excessive itching, burning or irritation
Varicose vein treatment
Research has shown that treatment of damaged veins in the leg can help to speed up the healing of leg ulceration. It can also prevent recurrence. Depending upon the results of your assessment, your specialist nurse will discuss having your veins treated and refer you to a vascular consultant if needed.
One of the available treatments involves having the troublesome vein injected. This can be done without having to stay in hospital. Further information about this can be found in a separate information leaflet GHPI0993 ‘Foam Sclerotherapy for varicose veins’.
More recently, a newer procedure called Radiofrequency Ablation (RFA) has become available. Please ask your specialist leg ulcer nurse for a copy of leaflet GHPI1498 ‘Radiofrequency Ablation (RFA) for varicose vein treatment’.
Diet
It is important for your general health to eat a well-balanced diet. This becomes more important when you are trying to heal your leg ulcer. Try to eat a diet which is well-balanced in proteins, vitamins and minerals, as these are the ingredients necessary for your body to heal. Nutritional supplements have not been shown to speed up healing so providing your diet is well-balanced, you will not need these.
If you are overweight, it is advisable to try and lose weight. This will help to reduce the stress on your circulation and help your ulcer to heal and remain healed.
Clothing
It is important to wear clothing that does not restrict the return flow of blood through the veins.
We would advise you to avoid wearing any kind of tight fitting under or over garments.
Your footwear needs to be well fitting, comfortable and safe. Be prepared to have to wear larger sized shoes while being treated with compression bandages. Most normal footwear can be worn with bandages. Lace ups or trainers that can expand easily to accommodate them are often better than slip on shoes. It is a good idea to bring these shoes with you when you attend for an assessment.
If footwear is a problem, alternatives can be discussed with the specialist nurse in the clinic.
Infection
All leg ulcers have bacteria in them, this is normal. In most cases they will not need treatment with antibiotics, as they do not affect the healing process. We would only recommend the use of antibiotics when there are clinical signs of infection. These include pain, swelling, warmth and redness to or around the wound. You may also feel unwell and have a temperature. If you suffer these symptoms at any time, you should contact your GP or community nurse. If out of normal surgery hours, contact your on-call district nurse or NHS 111 for advice.
Skin care
There are several skin problems associated with venous disease. The most troublesome of these is eczema. It is important to remember that compression therapy is also a treatment for this complaint.
Creams alone will not cure venous eczema. High elevation of the limb will relieve symptoms. Once your ulcer has healed, daily application of a non-perfumed moisturising cream and continuous wearing of your compression stockings will stop venous eczema in most cases.
Another common skin condition is staining. The brown stain is caused by the blood cells leaking into the skin due to the damaged veins. This is unfortunately permanent but can sometimes fade with time. It will however not get any worse if you continue to wear compression.
Hyperkeratosis is the over-formation of skin causing the leg to appear scaly. In most cases regular washing and application of moisturising cream can resolve this. Hyperkeratosis often appears to become worse when being treated in compression bandages. It is often helpful if your leg can be washed at least once a week during treatment. This will resolve once the treatment for your leg ulcer is completed and you are able to wash the limb more regularly.
When your ulcer has healed
Once your leg ulcer has healed, it is important to continue to control any problems with your veins and swelling in the legs. For this reason, it is advisable that you continue to wear compression on the affected leg in the form of a compression stocking or sock.
Your specialist or community nurse will be able to advise you regarding compression stockings or socks and will measure your leg(s) to make sure of the correct fit.
Further information about how best to look after your legs and reduce the risk of further recurrence of your ulcer can be found in a separate patient information leaflet; GHPI0698 ‘Leg ulcer prevention’. Please ask your specialist nurse for a copy.
Contact information
Gloucestershire Leg Ulcer Service is based at Cheltenham General Hospital and runs clinics across the county. You can contact the team in the following ways:
Gloucestershire Leg Ulcer Service
Tel: 0300 422 3480 (secretary)
Monday to Friday, 9:00am to 5:00pm
Voicemail messages can be left outside of these times if non-urgent.
Email: ghn-tr.legulcerserviceghnhsft@nhs.net
You can also find us on Facebook or Twitter