Vitrectomy surgery
The information on this page is a guide for patients and carers about vitrectomy surgery.
On this page
What is vitrectomy?
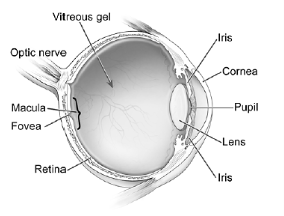
Vitrectomy is an operation to remove the clear gel (jelly), the vitreous humour, from inside the eye. The vitreous is found behind the lens and coloured iris. It is surrounded by and supports the retina.
Why do people need to have a vitrectomy?
Retinal detachment
A detached retina will usually cause progressive visual loss without treatment. The majority of cases need to be repaired on an urgent basis.
Macular hole or epiretinal membrane
The macula is the central area of retina used for fine vision such as reading text. A hole or membrane usually causes distortion of vision or blurred central vision.
Vitreous haemorrhage (bleeding)
Blood within the gel may cause visual dark swirls or misted vision. This can happen in conditions such as diabetes which can cause the growth of unhealthy fragile new blood vessels.
Eye trauma
Injuries that open the eye ball or pieces of metal entering the eye during accidents may require vitrectomy surgery to repair the damage.
Diagnostic
Taking a sample of the vitreous to examine it for infections or cancers, allows the correct treatment to be given.
Pre-assessment
Before your operation you will be sent an appointment for a pre -assessment appointment. If you are having a local anaesthetic, this is usually a telephone appointment with a member of the pre-assessment nursing team.
- Please have to hand a list of all your medications and allergies if you have any.
- Next of kin name and contact telephone number(s).
- Tell the nurse if you take medications to thin your blood.
If you take warfarin, you will be asked to visit your GP, 3 to 5 days before your surgery to have your INR checked.
You may also be invited for an appointment to come into hospital to take some measurements of your eyes called biometry. This is a painless scan of both eyes and is done by a member of the nursing team. The measurements are useful for the ophthalmologist as part of the surgery.
- Please bring with you a copy of your optician’s prescription for your current glasses to this appointment
If you develop any signs of an eye infection in the week before your surgery, please contact the hospital admissions team as your surgery will need to be cancelled until the infection resolves. The telephone number is at the end of this page.
Infection symptoms include a red, sticky eye.
If you are having the surgery under general anaesthetic- you will need to have a face-to-face appointment with a pre-assessment nurse in clinic.
How is the surgery performed?
Surgery is usually performed under local anaesthetic with the patient awake, but made very comfortable. Patients with severe anxiety may be offered sedation (to make them relaxed and drowsy) or occasionally a general anaesthetic (completely unconscious), although this may be limited by pre-existing medical conditions.
Your surgeon will discuss this with you before the operation and choose the most suitable option for you.
You will lay flat on a surgical couch, with a clear plastic drape over your face, to keep the surgical area sterile, which is lifted up to form a small ‘tent’. An air pipe will allow you to breath comfortably and prevent claustrophobia. You will not be able to see anything unnerving. Most patients will have no vision in the anaesthetised eye.
During the operation, your eye will remain in its natural position, and fine instruments will be inserted through key-hole wounds to gently remove the vitreous gel. This allows further treatments to the retina as required, and is often combined with cataract surgery if necessary. The procedure usually takes about 1 hour, but make take up to 2 hours, depending on the complexity. In most cases the key-hole wounds are self-sealing but occasionally a tiny dissolvable stitch is used to close them.
Is the vitreous gel replaced?
The vitreous gel is not needed in an adult eye and in most cases the eye will fill up with natural fluid (aqueous humour) over time.
In most procedures, the retina requires some support to help it heal properly. A temporary bubble is used to support the retina from the inside.
- Air bubble. This will cause your vision to be very blurred but will clear in 7 to 10 days.
- Gas bubble. Your vision will be very blurred with a gas bubble in the eye. Different medical gases may be absorbed over 2, 4 or 8 weeks, depending on the level or support required for the retina. Patients are given a bright wrist-band for the duration of this to remind them not to travel in an aeroplane or have a gas anaesthetic during this time.
- Silicone oil bubble. This provides longer-term support to the retina and is not absorbed naturally. Your vision will be blurred by the bubble but less so compared to air or gas. The majority of patients will have a second operation at a later stage to remove the oil.
Positioning after the operation
Most bubbles used in the eye will float upwards due to gravity. If the area affected is away from the top of your eye, you may be asked to position your head to allow the bubble to best support the affected area of the retina. Typically, this will be for a few days after the surgery and should be performed for 50 minutes in each hour to allow for comfort breaks. Positioning may vary between night and day-time to allow comfortable sleeping.
What happens after the surgery?
- Usually, the vision will be temporarily blurred depending on the bubble used within your eye. Permanent vision can be assessed when the bubble has been absorbed or removed. We recommend holding off opticians’ checks until 6 weeks after the surgery or when the bubble has gone (whichever is latest).
- Your eye might appear red and feel gritty or sore for 1 to 2 weeks. Pain relief and regular eye drops will help, these will be prescribed by your surgeon after the operation.
- Normal follow-up is in clinic around 1 week after the surgery, but this may vary.
Possible complications
Cataract development
Cataract development may be hastened in the months following vitrectomy surgery. Some patients will have cataract surgery performed at the same time, but this is not suitable in every case. Cataract surgery is a smaller procedure that can be performed as a day-case if it does develop after vitrectomy.
Retinal detachment
Retinal detachment is an uncommon complication after vitrectomy surgery (less than 2 in every 100 patients). For vitrectomy performed to treat retinal detachment, the success rate is above 80%.
Severe visual loss
Severe visual loss is very rare (1 in every 1000 patients) and may be related to severe bleeding or infection within the eye (endophthalmitis).
Contact us promptly if you notice
- Severe pain
- Suddenly reduced vision (gas bubbles will cause blurring, but vision will remain bright)
- An increasingly red eye
- Feeling of nausea or actual vomiting.
Contact information
If you any issues after surgery, please contact:
Eye triage
Tel: 0300 422 3578
Monday to Friday, 8:00am to 6:00pm
Saturday, 8:00am to 1:00pm
Outside of these hours, calls will be directed to the hospital switchboard.
Tel: 0300 422 22222
When prompted, ask to speak to the operator. You should then ask the operator to put you through to the on-call eye doctor.
If you have any queries about your treatment which are not covered on this page, please ask any member of the medical or nursing staff for advice.
Further information
Additional information about retinal surgery in the UK can be found at the following website:
British & Eire Association of Vitreoretinal Surgeons
Website: www.beavrs.org